Supplemental Material: Case series and reports of exposure to
advertisement
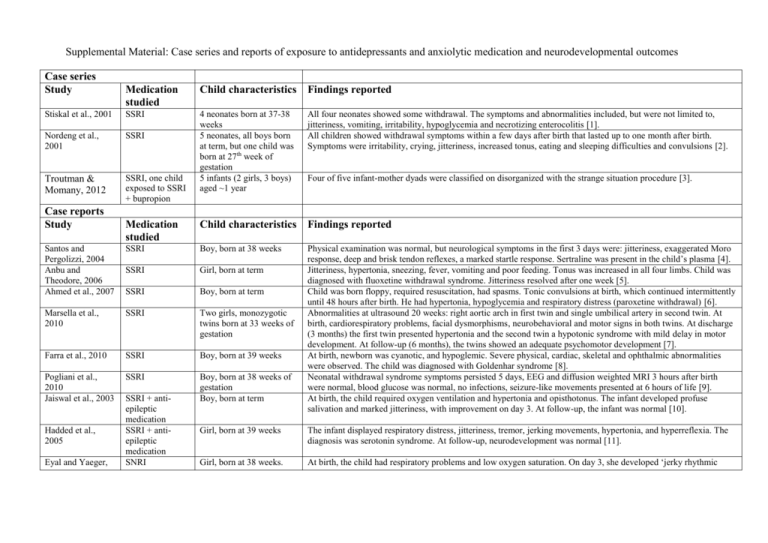
Supplemental Material: Case series and reports of exposure to antidepressants and anxiolytic medication and neurodevelopmental outcomes Case series Study Medication studied Child characteristics Findings reported Stiskal et al., 2001 SSRI Nordeng et al., 2001 SSRI All four neonates showed some withdrawal. The symptoms and abnormalities included, but were not limited to, jitteriness, vomiting, irritability, hypoglycemia and necrotizing enterocolitis [1]. All children showed withdrawal symptoms within a few days after birth that lasted up to one month after birth. Symptoms were irritability, crying, jitteriness, increased tonus, eating and sleeping difficulties and convulsions [2]. Troutman & Momany, 2012 SSRI, one child exposed to SSRI + bupropion 4 neonates born at 37-38 weeks 5 neonates, all boys born at term, but one child was born at 27th week of gestation 5 infants (2 girls, 3 boys) aged ~1 year Medication studied Child characteristics Findings reported Santos and Pergolizzi, 2004 Anbu and Theodore, 2006 Ahmed et al., 2007 SSRI Boy, born at 38 weeks SSRI Girl, born at term SSRI Boy, born at term Marsella et al., 2010 SSRI Two girls, monozygotic twins born at 33 weeks of gestation Farra et al., 2010 SSRI Boy, born at 39 weeks Pogliani et al., 2010 Jaiswal et al., 2003 SSRI Boy, born at 38 weeks of gestation Boy, born at term Physical examination was normal, but neurological symptoms in the first 3 days were: jitteriness, exaggerated Moro response, deep and brisk tendon reflexes, a marked startle response. Sertraline was present in the child’s plasma [4]. Jitteriness, hypertonia, sneezing, fever, vomiting and poor feeding. Tonus was increased in all four limbs. Child was diagnosed with fluoxetine withdrawal syndrome. Jitteriness resolved after one week [5]. Child was born floppy, required resuscitation, had spasms. Tonic convulsions at birth, which continued intermittently until 48 hours after birth. He had hypertonia, hypoglycemia and respiratory distress (paroxetine withdrawal) [6]. Abnormalities at ultrasound 20 weeks: right aortic arch in first twin and single umbilical artery in second twin. At birth, cardiorespiratory problems, facial dysmorphisms, neurobehavioral and motor signs in both twins. At discharge (3 months) the first twin presented hypertonia and the second twin a hypotonic syndrome with mild delay in motor development. At follow-up (6 months), the twins showed an adequate psychomotor development [7]. At birth, newborn was cyanotic, and hypoglemic. Severe physical, cardiac, skeletal and ophthalmic abnormalities were observed. The child was diagnosed with Goldenhar syndrome [8]. Neonatal withdrawal syndrome symptoms persisted 5 days, EEG and diffusion weighted MRI 3 hours after birth were normal, blood glucose was normal, no infections, seizure-like movements presented at 6 hours of life [9]. At birth, the child required oxygen ventilation and hypertonia and opisthotonus. The infant developed profuse salivation and marked jitteriness, with improvement on day 3. At follow-up, the infant was normal [10]. Case reports Study Hadded et al., 2005 Eyal and Yaeger, SSRI + antiepileptic medication SSRI + antiepileptic medication SNRI Four of five infant-mother dyads were classified on disorganized with the strange situation procedure [3]. Girl, born at 39 weeks The infant displayed respiratory distress, jitteriness, tremor, jerking movements, hypertonia, and hyperreflexia. The diagnosis was serotonin syndrome. At follow-up, neurodevelopment was normal [11]. Girl, born at 38 weeks. At birth, the child had respiratory problems and low oxygen saturation. On day 3, she developed ‘jerky rhythmic 2008 Hoppenbrouwers et al., 2010 SNRI Boy, born at 41 weeks of gestation Frey et al., 1999 TCA (pregnancy and postpartum) Boy, born at term Bloem et al., 1999 TCA Boy, born at term Sokolover et al., 2008 TCA Alehan et al., 2008 Benzodiazepine (first trimester) + SSRI (second and third trimester) Twins, boys, monozygotic, born at 35 weeks Girl, born at 41 weeks movements’. EEG showed nonspecific encephalopathic finding. The child was diagnosed with tremors and neonatal seizures associated with neonatal behavior syndrome. At 2 years, the child was healthy with normal neurobehavioral development [12]. The child had tachypnea, feeding difficulties, mild withdrawal, and a neonatal infection. Restlessness, tachypnea, higher Finnegan scores, and episodes of extensor limb posturing and severe agitation were observed. EEG results were judged as ‘suspect for epilepsy’ [13]. At 9 days the infant showed poor sucking, swallowing problems, muscle hypotonia, and vomiting. He had lost weight, was drowsy and jaundiced. Breastfeeding was discontinued, because doxepin was detected in breast milk and in the child’s plasma. Two days later he was asymptomatic and was discharged [14]. Two days after birth the child was jittery and showed startling impulses, simultaneous and symmetrical jerks of arms and legs. The jerks could be provoked by touch or auditory stimuli, and stopped by briefly stabilizing the limb. Ultrasound brain scans and EEG were normal. The diagnosis was a generalized, stimulus sensitive, status myoclonus. Examination three weeks later was normal, except for mild jitteriness in response to touch [15]. At birth, mild hypotonicity and poor sucking were noted in one twin, but physical and neurological examinations were normal. On day 3, both twins showed hypothermia, and thermal instability until the 10 th day of their life. Follow-up at 4 months showed normal growth and development [16]. Infant was jittery, hypertonic with oculogyric crises, vomited and showed poor feeding. The child was diagnosed with fluoxetine withdrawal, which persisted for 6 weeks. At 3 years old, the child had mild mental retardation and microcephaly [17]. Abbreviations: EEG: electroencephalogram; MAO: monoamine oxidase inhibitor; MRI: magnetic resonance imaging; NDRI: norepinephrine/dopamine reuptake inhibitor; SNRI: serotonin/norepinephrine reuptake inhibitor; SSRI: selective serotonin reuptake inhibitor; TCA: tricyclic antidepressant. References: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. Stiskal JA, Kulin N, Koren G, Ho T, Ito S (2001) Neonatal paroxetine withdrawal syndrome. Archives of Disease in Childhood: Fetal and Neonatal Edition 84:F134-F135 Nordeng H, Lindemann R, Perminov KV, Reikvam A (2001) Neonatal withdrawal syndrome after in utero exposure to selective serotonin reuptake inhibitors. Acta Paediatrica, International Journal of Paediatrics 90:288-291 Troutman BR, Momany AM (2012) Use of selective serotonin reuptake inhibitors during pregnancy and disorganised infant-mother attachment. Journal of Reproductive and Infant Psychology 30:261-277 Santos RP, Pergolizzi JJ (2004) Transient neonatal jitteriness due to maternal use of sertraline (Zoloft). Journal of perinatology : official journal of the California Perinatal Association 24:392-394 Anbu AT, Theodore A (2006) Fluoxetine withdrawal syndrome in the newborn. Indian Pediatr 43:66-69 Ahmed M, Parameshwaran A, Swamy P (2007) Neonatal convulsions secondary to paroxetine withdrawal. J Pak Med Assoc 57:162 Marsella M, Ubaldini E, Solinas A, Guerrini P (2010) Prenatal exposure to serotonin reuptake inhibitors: a case report. Ital J Pediatr 36:27 Farra C, Yunis K, Mikati M, Yazbeck N, Majdalani M, Awwad J (2010) Goldenhar syndrome associated with prenatal maternal Fluoxetine ingestion: Cause or coincidence? Birth Defects Res A Clin Mol Teratol 88:582-585 Pogliani L, Schneider L, Dilillo D, Penagini F, Zuccotti GV (2010) Paroxetine and neonatal withdrawal syndrome. BMJ Case Rep 2010 Jaiswal S, Coombs RC, Isbister GK (2003) Paroxetine withdrawal in a neonate with historical and laboratory confirmation. Eur J Pediatr 162:723-724 Haddad PM, Pal BR, Clarke P, Wieck A, Sridhiran S (2005) Neonatal symptoms following maternal paroxetine treatment: serotonin toxicity or paroxetine discontinuation syndrome? J Psychopharmacol 19:554-557 Eyal R, Yaeger D (2008) Poor neonatal adaptation after in utero exposure to duloxetine. Am J Psychiatry 165:651 Hoppenbrouwers CJ, Bosma J, Wennink HJ, Hilgevoord AA, Heres M, Honig A (2010) Neonatal seizures on EEG after in utero exposure to venlafaxine. Br J Clin Pharmacol 70:454-456 Frey OR, Scheidt P, Von Brenndorff AI (1999) Adverse effects in a newborn infant breast-fed by a mother treated with doxepin. Annals of Pharmacotherapy 33:690-693 Bloem BR, Lammers GJ, Roofthooft DW, De Beaufort AJ, Brouwer OF (1999) Clomipramine withdrawal in newborns. Arch Dis Child Fetal Neonatal Ed 81:F77 Sokolover N, Merlob P, Klinger G (2008) Neonatal recurrent prolonged hypothermia associated with maternal mirtazapine treatment during pregnancy. Can J Clin Pharmacol 15:e188-190 Alehan F, Saygi S, Tarcan A, Gurakan B (2008) Prolonged neonatal complications after in utero exposure to fluoxetine. Journal of Maternal-Fetal and Neonatal Medicine 21:921-923