Almas psychiatry
advertisement
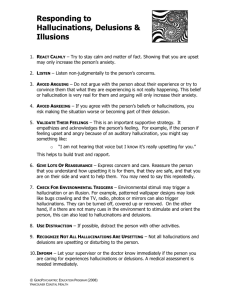
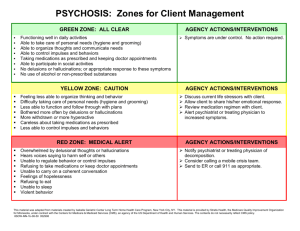
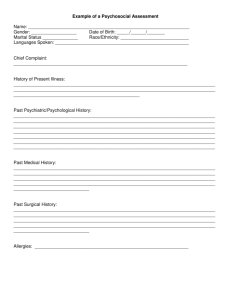
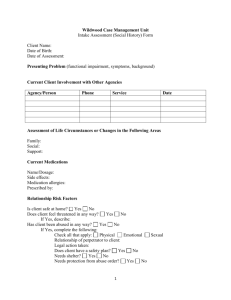
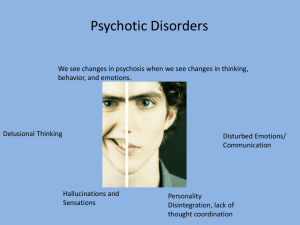
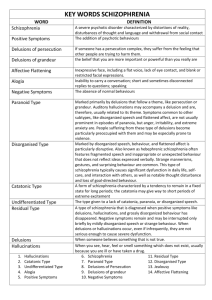
Psychiatry in General Practice Dr Almas Malik ST2 GPVTS Aims • MSE • Case scenario • Risk • Perinatal psychiatry • Schizophrenia mx • Ward interaction with PD • Bipolar – when to refer • Screening Mental State Exam A+B: eye contact, posture, psychomotor Speech: rate, volume, tone Mood: subjectively and objectively Thoughts: content, flow, preoccupied, obsessive, delusions Perception: hallucinations Risk Insight Case 1 • 39 yrs female, south Asian. Married, housewife, 2 • • • • • children 5 + 8. Previous consults non-specific hand pain + pre-menstrual sx’s + menorrhagia – (both investigated) Presents with hand pain + heavy periods Not sleeping, tired all the time, husband doesn’t do anything Hand pain is so bad I want to kill myself I can’t cope with looking after the children Doctor please help me! Assessing Risk To self: superficial cutting, suicide, self-neglect From others: Financial, Sexual, Physical. Contraception To others: children in home, partners, family Questions: thoughts of wanting to end their life, attempts to end their life, plans to end their life – what, when, how, plans for future, anything that would stop them taking their own life – children. Superficial cutting – frequency, intoxicated while harming Past history of violence, suicide attempts, criminal records • Social: home alone all day. Spends her time doing housework and looking after children. Doesn’t socialise, no friends. Husband works in post office and pastor. No alcohol or drugs • Why now – psychosocial triggers Management of depression • Assess risk + function • Admission or manage in primary care • Crisis plan to all patients: A+E, Samaritans + SLAM 24 hour line • Non-pharmacological: self-help CBT Moodgym, MIND, physical activity, regular reviews, SUN project – emotional support group, Touchstone Centre – group and individual psychotherapy • Pharmacological – Moderate - severe 1. SSRI’s – citalopram 20mg od (r/w in first 2 weeks) 2. Different SSRI – sertraline 50mg od 3. Mirtazepine 30mg od (if sleep disturbance) 4. Venlafaxine 75mg od Prevention – coping, social support, relaxation, exercise Perinatal psychiatry • Baby blues – in first week, lasting few days. No tx • Post-natal depression – in 6 months. Sertraline or paroxetine, mother and baby unit • Puerperal psychosis First 2 weeks, mood disturbance + delusions + hallucinations. Refer urgently. antidepressant’s in pregnancy • Sertraline preferred • TCA’s lower risks in pregnancy, but dangerous in O/D • Paroxetine in first trimester fetal heart defects - avoid • Risk of mild, self-limiting withdrawal sx’s in neonate with all anti-depressants Management schizophrenia Medication is mainstay of tx single agent Risperidone Olanzapine – weight gain, cardiovascular risk, diabetes risk Role of CBT – hallucinations + delusions, improve social functioning Family therapy Refer – risk issues, acutely distressed, decline of functioning Interesting interaction • 39 yr old female, stood in corridor with bleeding arm • • • • • from superficial cuts. Benzodiazepine reduced Feeling anxious, boyfriend’s mum’s funeral coming up. Wanted to support boyfriend but funeral was bringing back memories of her own mother’s death. Couldn’t cope with this additional stressor with current admission + medication changes Wants benzodiazepine now as stressed and can’t cope Bereavement counselling offered. Advised to speak to her bf about how she was feeling. Commented disliked Dr.. Seen a few times in the week, wanted to be seen more Burdened, avoiding patient. PD In GP • Splitting • Repeated - ‘heart-sink’ • Dependent nature • Impulsive • Instant gratification • Poor-coping strategies Management PD • Medication has no role • Help understanding of their diagnosis • Talking therapies • Touchstone group therapies to understand actions and feelings • SUN project – coping skills and support • Negotiate how often patient is seen • Admissions detrimental Bipolar Refer – • acute relapses, risk, decline in functioning, non- compliance • Meds: antimanic – antipsychotics, valproate, lithium Preventing relapse: • Patient education – recognise early symptoms of relapse and seek help. Coping strategies • Sleep hygiene, regular lifestyle. Shift work, flights ax time zones • Support during significant life events ‘ I think of the future it seems so bleak I wish I could retain my high when at its peak But I always seem to drop face first and hit the concrete I feel like a prisoner of my own mind I just wanna escape another identity, place and time Anything to stop me feeling so confined I used to think the answer would be in a bottle of wine I feel so guilty for the burden placed on my daughter and hate myself for having this mental disorder I don’t want my daughter to care for her mum I just wanted to perfect life for her I have secret fears for her sanity as they say an illness like this can be hereditary Its a lonely feeling knowing you’re so misunderstood I just want somebody to listen and fully understand Offer me comfort and the support of a helping hand Remind me I’m not alone and God still has a plan Please Lord don’t let me slip from the grasp of your hand’ MH screening At risk groups: Chronic medical problems Women – young, pregnancy, mother’s, menopause Carers Minority ethnic groups Relapses: Non-compliance Social triggers References • NICE guidelines • CSK website • http://www.rcpsych.ac.uk/