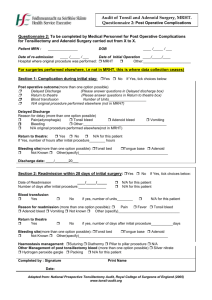
postoperative complications
advertisement

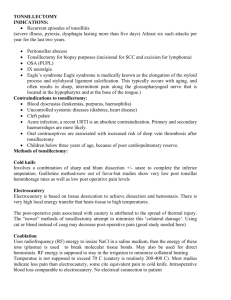
Adapted from John Hunter guideline 8.2 (Australia) for PCEA Tumutumu Hospital Kenya GUIDELINE OBJECTIVE: This guideline aims to assist clinical staff to provide effective care to paediatric patients following a tonsillectomy/ adeno-tonsillectomy by providing guidelines on: Recognition and management of primary haemorrhage Recognition and management of airway compromise Effective pain relief Safe maintenance of hydration Minimisation of post-operative nausea and vomiting Information on discharge The three principal post-operative complications of tonsillectomy/adenotonsillectomy are: 1. Bleeding – primary haemorrhage, 2. Airway obstruction 3. Fluid mismanagement – iatrogenic hyponatraemia Factors associated with an increased risk of post tonsillectomy/adenotonsillectomy haemorrhage include: Coagulopathy Increasing age of child Quinsy (peri-tonsillar abscess) tonsillectomy Factors associated with an increased risk of post tonsillectomy/adenotonsillectomy airway obstruction include: Increasing Respiratory Disturbance Index (RDI), especially in Rapid Eye Movement (REM) phase – that means events such as apnoea, hypoventilation, respiratory distress that occur during sleep Severe Obstructive Sleep Apnoea (OSA) March 2015 For review March 2016 Cranio-facial syndromes, mucopolysaccharidoses, achondroplasia, Pierre Robin sequence, Down syndrome, some neuromuscular diseases Factors associated with an increased risk of post tonsillectomy/adenotonsillectomy iatrogenic hyponatraemia include: Using solutions other than Normal Saline or Hartmann’s Solution in the first 24 hours (other solutions contain too much water for the immediate post-operative period) vomiting CLINICAL GUIDELINES: Considerations for post-op Paediatric Intensive Care Unit (PICU) admission. Tumutumu does not have an intensive care unit. Therefore nursing and medical staff to seek clarification from paediatric and surgical senior staff on appropriate care post tonsillectomy in addition to guidelines set out below, as well as consideration for tonsillectomy to be done in a centre that does have a PCIU: Isolated Respiratory Disturbance Index (RDI) in Rapid Eye Movement (REM) sleep greater than 60. RDI in REM less than 60 plus consideration of - a syndrome likely to be complicated by airway obstruction (eg cranio-facial anomalies, mucopolysaccharidoses, achondroplasia, Pierre Robin sequence, Down syndrome), or - age less than 24 months, - weight for height Z score less than -2SD or MUAC <12.5cm - significant neuromuscular disease or respiratory compromise, or significant central component > 40%. i.e. not obstructive – can be complicated by troublesome hypoventilation Severe OSA as determined by a sleep study- PSG Complex cyanotic/ congenital heart disease After discussion amongst Surgeon, Anaesthetist, and Intensivist March 2015 For review March 2016 1. Observations: (unless ordered otherwise) 1.1Pulse, Respirations and Oxygen Saturations every 15 minutes until “Post –Op Stable” as defined by the criteria below. Vital signs monitoring should be supervised by a trained nurse and must be checked against the normal parameters for children according to age category (poster of paediatric vital signs at nurses station in ward 2 for reference). 1.2 Blood pressure as directed by the surgeon “Post –Op Stable” is defined as: awake protecting their airway with adequate analgesia not vomiting haemodynamically stable (vital signs in normal parameters) Ideally a patient should be completely “Post-op Stable” prior to transfer back to ward, if does not meet all the above criteria, inform the surgical team and continue vital signs every 15 minutes until stable. Patients MUST be transferred with all post-operative instructions, drug chart and IV prescription chart and vital signs documented in patient notes by the surgeon and anaesthetist. Do not transfer the patient back to the ward without them. Post Op Stable further monitoring: (unless ordered otherwise) 1.4 Record observations vital signs chart including pulse, oxygen saturations and respirations half hourly for a further 4 hours then, 1.5 Pulse and respirations hourly for 20 hours, or for as long as indicated by the medical officer, then 4 hourly till discharge, 1.6 Temperature 4 hourly, 1.7 Blood pressure 4th hourly for children > 12 years. Call surgical team if oxygen saturations reading < 92% (ensure trace is good). 1.8 Re-evaluate child periodically to determine whether additional treatment/ supports are required eg. oxygenation, positioning March 2015 For review March 2016 * Report abnormal observations promptly to the appropriate medical officer* 2 Observe for: 2.5 Behavioural disturbances eg. odd sleeping position, restlessness, agitation, sleepiness, and irregular breathing pattern - these indicators may be due to hypoxia. 2.6 Frank bleeding from the nose or mouth 2.7 Excessive swallowing or Frequent clearing of throat 2.8 Tachycardia 2.9 Pallor and sweating 2.10 Nausea and vomiting - inspect vomitus for fresh blood IN AN EMERGENCY CALL THE , Medical Officer, PAEDIATRICIAN and SURGEON 3 Pain Management Rationale: The literature suggests: children may experience significant pain after tonsillectomy regular pain relief is more effective than prn regular paracetamol is the mainstay of effective analgesia 3.1 Pain Management: Paracetamol doses should be calculated based on body weight Oral administration of paracetamol is preferred, but the rectal and IV routes may be used for acute, short- term treatment Other analgesics may be prescribed by the anaesthetist in liaison with the Surgical team. Ibuprofen (Nurofen) and other non-steroidal anti-inflammatory drugs should be avoided unless specifically prescribed due to risk of bleeding. March 2015 For review March 2016 Refer to regular and PRN medication charts. NB- Opioids to be used with caution Children with a history suggestive of sleep apnoea are particularly sensitive to the respiratory depressant effects of opioids and sedative agents In the ward areas, note that the restless child may be hypoxic due to blood loss or respiratory depression/sleep apnoea Check pre-op and anaesthetic record for medications already given, and their timing, before administering regular or PRN analgesics. 4 Fluids- Choice of IVF replacement therapy is very important to avoid iatrogenic Hyponatraemia 4.1 Outside of PICU Hartmann’s Solution or Normal Saline only are to be administered in the first 24hrs post op. Note: Hartmann’s Solution has a number of medication incompatibilities so check any additives. 4.2 Encourage oral fluids and document all intake and output on a fluid balance chart. 5 Medications for Nausea/Vomiting: 5.1 If nausea or vomiting persists, the child is to be reviewed by the Surgeon/ Medical Officer before discharge. 6 Indicators for patient discharge: 6.1Tolerating soft diet, advancing to regular diet. 6.2 Adequate oral intake – according to age and underlying medical conditions (or as advised by the Surgeon). 6.2 Post operation void has occurred before discharge. 6.3 Parent/carers are confident to take their child home. 7 Discharge Plan: March 2015 For review March 2016 Ensure parent / carer has: 7.1Discharge information 7.2 Follow up appointment 7.3 Discharge prescription (eg for antibiotics) if ordered 7.4 Contact phone number- to direct concerns Discharge Criteria: Vital signs are stable and within normal limits Tolerating fluid, advancing to normal diet Nil vomiting Has voided post operatively Pain controlled by oral analgesia Information on post-op. care & contact telephone numbers provided to carers. March 2015 For review March 2016