File
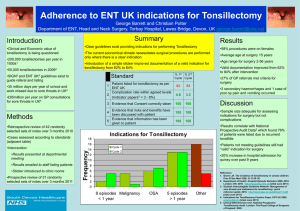
advertisement

CHICAGO-In this corner, cold tonsillectomy. And in the opposite corner, hot tonsillectomy. In the middle, some evidence-based data and lots of experience-based opinion supporting both techniques. While no one is going to be coming out swinging to settle this dispute, one would probably be hard pressed to find a more polarizing professional issue for otolaryngologists. Perhaps that is putting it a little dramatically, but the consensus regarding the best tonsillectomy technique is that there is no consensus. I think intracapsular tonsillectomy is best done on small children with obstructive sleep-disordered breathing. - -Peter Koltai, MD A distinguished panel of experts, with varying preferences when it comes to tonsillectomy technique, gathered to discuss the data and relate their experiences in a special session presented by the American Society of Pediatric Otolaryngology here at the Combined Otolaryngology Spring Meetings (COSM). The related issues at the heart of the debate involve which technique is better when it comes to primary and secondary bleeding, operative time, postoperative morbidity (pain and infection), and risk of recurrence. There are a lot of questions that need to be answered before we will be able to resolve some of the issues and determine the best technique to do tonsillectomy and adenoidectomy, said session moderator Brian Wiatrak, MD, of the Department of Otolaryngology at the Children's Hospital of Alabama in Birmingham. There have been a lot of publications that, scientifically, may be lacking in terms of some of the statistical techniques that were used. I think there needs to be a careful examination of the publications that are sent to journals in terms of how much evidence is really there and how the statistical analysis is done. COLD STEEL Unfortunately, some otolaryngologists think of cold steel tonsillectomy as crude and bloody but, like a marine in hand-to-hand combat, it's fairly effective and really can be quite elegant, said Anna Messner, MD, Associate Professor of Otolaryngology and Pediatrics of the Lucile Salter Packard Children's Hospital at Stanford University (Calif.). There are quite a few programs now where the residents actually never learn anything about cold technique. Dr. Messner admits that the literature predominantly favors hot technique with regards to intraoperative blood loss, pointing to a 2003 review article that looked at six studies comparing primary hemorrhage of the two techniques. In a study published more recently, they also found less blood loss with cautery. The one caveat with this study, though, is they did not use the same adenoidectomy technique, she said. In the cautery group, they used suction cautery adenoidectomy; in the cold group they used a curet, so that would tend to increase the cold blood loss a little bit more. In that same review, she noted, there were three papers that compared operative time, with two of the three reporting a longer operative time for the cold technique, and one with a shorter operative time. Overall, cold probably does take a little bit longer, but that probably has a lot to do with the surgeon's experience. But when we're thinking about operative time, are we talking about it in terms of being clinically significant or, realistically, financially significant? she said. If that extra amount of time pushes you into the next fifteen-minute increment for your OR time, that can be incredibly expensive. On the plus side, two wires for a snare cost approximately $1.63, which is, by medical standards, an incredible bargain. What about postoperative hemorrhage, morbidity, and recurrence? You do probably have, according to the latest data, an improved postoperative hemorrhage rate; you definitely have decreased postoperative morbidity and there's less risk of recurrence of the problem, Dr. Messner said. My conclusion is, even though it's old and not very sexy and doesn't require a lot of equipment, go with the cold. ELECTROCAUTERY When evaluating tonsillectomy technique, there is probably less evidence-based medicine (EBM) reflected in the current literature, and more of a completely different EBM-emotionally biased medicine, that isaccording to Charles Myer III, MD, Professor of Otolaryngology and Director of the Hearing Impaired Clinic at Children's Hospital Medical Center in Cincinnati, Ohio. There's a preponderance of both evidence and emotion on both sides as relates to cost, hemorrhage, and pain, he said, admitting that his thoughts on the subject are probably no less emotionally biased that what's in the literature. Dr. Myer believes that, in light of there being no clear-cut answers to the hot-cold question, surgeons must rely on their own experience to decide which technique is best for their patients. When you have something that works, and in my case it's electrocautery, stick with it, he said. Sometimes I think people make a decision to change just for the sake of change. We certainly can't be staid in our approach to things, as nothing new will be developed if we're not open to change, but the data must be supportive of those changes that we choose to make. And, for Dr. Myer, the data just isn't there to convince him that there is any compelling reason for him to change from a technique that he is comfortable with and has been performing for the past 20 years. Electrocautery is historically sound, relatively easy, effective, comfortable both for the surgeon and the staff, he said. It also has a predictable set of complications and I don't think any different technique measures up to this. INTRACAPSULAR click for large version Figure. A microdebrider can be used to perform intracapsular tonsillectomy. In 1930, physician Robert Fowler described the modern tonsillectomy as removing the whole tonsil and nothing but the tonsil, which made a lot of sense in the pre-antibiotic era when there was concern that subtotal resection could get re-infected There were ample anecdotes from the tonsillotomy era about the regrowth of tonsils and the persistence of disease, said Peter Koltai, MD, Professor of Otolaryngology and Pediatrics at the Stanford University Medical Center. However, subsequent to the development of total tonsillectomy, it has become evident that there's no such thing as a painless tonsillectomy that never bleeds. The evidence, as it stands today, does support no significant difference in primary bleeding for Coblation in both complete and partial tonsillectomy…[and] also finds no significant difference in delayed bleeding, and pain in general is considered to be far less with Coblation. - -Udayan Shah, MD But about ten years ago, Dr. Koltai and his colleagues began to contemplate whether or not there was a better way. The general concept of the intracapsular tonsillectomy was derived from the case of a specific child-an 11-month with severe obstructive sleep apnea and very large tonsils who had failed to respond to antibiotic therapy and steroids. Electrocautery is historically sound, relatively easy, effective, comfortable both for the surgeon and the staff. It also has a predictable set of complications and I don't think any different technique measures up to this. - -Charles Myer III, MD We believed that a tonsillectomy and adenoidectomy would resolve the problem, but we all know how challenging regular T&A is to an 11-month old, so we considered a minimally invasive alternative, he said. In 1994, Joe Krespi had introduced a procedure called the laser-assisted serial tonsillectomy. After the procedure, these kids would leave the office after local anesthesia and seemed to do very well with reduced bleeding, Dr. Koltai said. Based on this new capsule-sparing insight and his previous experience using the microdebrider for adenoidectomy, Dr. Koltai decided to use that instrument to treat that 11-month-old patient and found that the child had a dramatic and rapid recovery. That was the beginning of intracapsular tonsillectomy. click for large version Figure. The coblation T&A wand can be used to ablate tonsil tissue and obtain hemostasis. Since that time, Dr. Koltai has undertaken three separate studies looking at the effect of intracapsular tonsillectomy. The results of those studies suggested fewer days to recovery and less analgesia, significantly reduced pain, and a significantly lower rate of dehydration and readmission to the hospital compared to total tonsillectomy. The concern about regrowth of the remnant and subsequent tonsillitis, however, is legitimate, he admitted. We acknowledge the problem and recognize the controversy, but propose that, today, most tonsillectomies are done for hypertrophy and not for infection, and less bleeding and lower bleeding rates do have a positive value, he said. Personally, I think intracapsular tonsillectomy is best done on small children with obstructive sleep-disordered breathing. We perform with the microdebrider, but believe that coblation is just as elegant and just as efficacious. COOLER ABLATION=COBLATION A recent survey of the American Society of Pediatric Otolaryngologists found that 16 percent of ASPO members use Coblation for tonsillectomy (Shah UK. What surgeons want in a tonsillectomy instrument: Results of an ASPO member survey. Poster presentation at the Annual Meeting of ASPO, Chicago, IL, May 21, 2006). Coblation is the brand name for the application of plasma-mediated ablation to soft tissue, which results in cooler tissue ablation, therefore the moniker: Coblation. Coblation has been a technology in evolution, with the controller and handpiece design progressively being better incorporated with integrated cables and tubing, said Udayan Shah, MD, Attending Surgeon and Director of the Otolaryngology Innovative Technologies Program at the Children's Hospital of Philadelphia (Pa.), and Assistant Professor of Otorhinolaryngology-Head and Neck Surgery at the University of Pennsylvania School of Medicine. The first device for tonsillectomy using plasma-mediated ablation was the plasma wand, which was introduced in 1998. He said the instrumentation has come a long way since then, and today, with better devices and more experienced surgeons, the evidence in the literature does overall support the use of Coblation for complete and partial tonsillectomy, for excision and intraoperative hemostasis. The evidence, as it stands today, does show that there is no significant difference in primary bleeding for Coblation in both complete and partial tonsillectomy compared with monopolar and cold techniques, he said. The bulk of the evidence also finds no significant difference in delayed bleeding, and pain in general is considered to be far less with Coblation. He said there are some questions, though, that still need to be answered. I think the economics do need to be addressed, and the question of regrowth following partial Coblation tonsillectomy needs to be answered as well, Dr. Shah said. Continued careful refinement, application, and investigation of Coblation technique and instrumentation, most likely involving multicenter cooperation, is going to be required to generate sufficient power in clinical studies to answer the questions that surgeons care most about according to the recent survey of ASPO members: Is it safe and will it reduce post-op hemorrhage? THE DATA Answers to many of the questions surrounding both hot and cold techniques may be forthcoming. Unfortunately, those answers may not be the ones needed to lay the great tonsillectomy debate to rest once and for all, according to David Albert, MD, a pediatric otolaryngologist at Great Ormond Street Hospital for Sick Children in London, UK. Dr. Albert's institution is one of many across the United Kingdom that participated in the much anticipated National Prospective Tonsillectomy Audit, which included data on nearly 40,000 tonsillectomy procedures performed across England and Ireland. If you look at the data regarding bipolar versus cold steel, there is a slightly lower risk of primary hemorrhage with bipolar, Dr. Albert said. But if you look at secondary hemorrhage, the risk is five times greater. If you look at monopolar, there are similar slightly reduced rates of primary but considerably higher secondary hemorrhage, and these are all highly statistically significant. click for large version Figure. Cold steel tonsillectomy offers the most economic choice of equipment-two wires for a snare (pictured) cost approximately $1.63. Although the audit may be the most comprehensive set of data exploring tonsillectomy technique to date, Dr. Albert said physicians should not be too quick to change from their current techniques. Unfortunately, some otolaryngologists think of cold steel tonsillectomy as crude and bloody but, like a marine in hand-to-hand combat, it's fairly effective and really can be quite elegant. - -Anna Messner, MD Before any of you consider changing techniques, you should perhaps consider your own data, he said. A lot of these techniques have steep learning curves. When I came to the decision for my own son who needed a tonsillectomy, I didn't choose the technique, I chose the surgeon.