File - Staff Training for Glenelg Community Hospital
advertisement

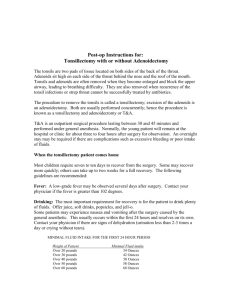
GLENELG COMMUNITY HOSPITAL INC Adenotonsillectomy Learning Package Name_____________________________________________RN/EN Date___________________________ Department_____________________ Return this Learning Package to Staff Educator for marking and a certificate 1 INTRODUCTION This self directed package is designed to assist nurses to become proficient in the care of an infant, child or adolescent and adult, who has had an Adenotonsillectomy. This package enables you to work through the skills at your own pace. OBJECTIVES On completion of the learning package you will be able to: KNOWLEDGE Describe the Paediatric airway anatomy and physiology Outline the definition of Adenotonsillectomy Describe the indications for Adenotonsillectomy Identify complications following an Adenotonsillectomy and state the actions required if these occur SKILLS Give total care for an infant, child or adolescent, or adult who has had an Adenotonsillectomy in a safe environment Evaluate respiratory status ATTITUDE Appreciate the need for staff to be competent in airway management before giving care to an infant, child or adolescent or adult who has had an Adenotonsillectomy Provide education to staff, patients and their families on care following Adenotonsillectomy. RELATED CONCEPTS Paediatric growth and development Paediatric respiratory assessment Respiratory anatomy and physiology Oxygen therapy Cardiopulmonary Resuscitation Infection Control practices Surgical nursing 2 ANATOMY AND PHYSIOLOGY The pharynx can be considered to be a muscular tube that connects the oral and nasal cavities with the oesophagus and larynx. While rather simple at first glance, the action of swallowing is considerably complex, requiring closure of the nasopharynx, closure of larynx propulsion of liquids and solids into the proximal oesophagus without aspiration into the tracheas and lungs. The pharynx can be divided into three parts: The boundaries of the nasopharynx are the skull base (basisphenoid) above and the soft palate below. The adenoid tissue is positioned in the midline of the posterior nasopharyngeal wall and is not visible through the mouth. Along with the tonsils, it makes up the major portion of the pharyngeal lymphoid tissue termed Waldeyers ring. The blood supply to the adenoid tissue arises from the ascending pharyngeal and sphenopalatine arteries. Branches of IX and X provide sensory innervation and are responsible for the referred pain to the ear/throat with adenoid infection. The oropharynx runs from the soft palate and palatal folds to the epiglottis. Tonsils (palatine and lingual) and adenoids are a collection of lymphoid tissue that helps the body fight infection. The palatine tonsils (commonly and from herein referred to as the” tonsils”) are located on either side of the oropharnyx. The palatine tonsils are visible at the back of the throat. The lingual tonsil lies over the posterior base of the tongue. The tonsillar branch of the facial artery provides the majority of the blood supply to the tonsils. In most people, the internal carotid artery lays two centimeters posterolateral to the deep surface of the tonsil. The nerve supply of the tonsils arises from IX and some branches of lesser palatine nerve via sphenopalatine ganglion. The hypopharynx begins at the epiglottis and extends to the level of the cricoid cartilage or the beginning of the oesophagus. At this point there is a muscle (cricopharyngeous) that closes off the pharynx form the oesophagus. The trachea projects upwards and backwards, to open into the front wall of the hypopharynx. At this junction the trachea forms the larynx. 3 Image of lateral view of the pharyngeal structures (Reference http://health.bwmc.umms.org/imagepages) Image of location of the tonsils and adenoids (Reference www.picsearch.com) 4 ADENOTONSILECTOMY DEFINITION Adenoidectomy and tonsillectomy, or Adenotonsillectomy (the removal of both the adenoids and the tonsils) is one of the most frequently performed surgical procedures in children. Studies have shown the greatest frequency of these operations lies between the ages of 4 and 8 years and between the ages of 13 and 23 years. INDICATIONS ADENOID Symptoms that indicate enlarged, obstructing adenoids that may benefit from an adenoidectomy include: The triad of hypo-nasality, snoring and mouth breathing Recurrent purulent rhinorrhea Post-nasal drip Chronic sinusitis Chronic middle ear effusions Persisting symptoms following medical therapy e.g. antibiotics Dental malocclusion or oro-facial growth disturbance Adenoid size may be graded. This grading refers to the observed size of the adenoid with respect to obstruction of the choanae. TONSIL The indications for a tonsillectomy are: Tonsillar hyperplasia causing upper airway obstruction and obstructive sleep apnoea Recurrent acute tonsillitis Recurrent peritonsillar abscess (there is a 10-20% chance of recurrence within 12 months, so most advocate removal of the tonsils after two episodes) Chronic tonsillitis (characterized by the triad of tonsilloliths, erythema of the tonsillar fauces, and enlarged cervical lymph nodes) Dysphasia due to tonsillar hyperplasia Dental malocclusion due to adversely affected orofacial growth Unilateral tonsil enlargement, presumed neoplastic) Brodsky, Moore and Stanievich describe as assessment scale for tonsillar hyperplasia. This scale is based on a percentage of obstruction. Another less frequently used method of grading is; - grade 1- tonsils were those lying lateral to the tonsillar fauces grade 2- at the level of the fauces grade 3- medial to the fauces but not to midline grade 4 –touching at the midline 5 Image of hyperplasia of tonsils Image of hyperplasia of tonsils 6 Image of mononucleosis Image of streptococcus infection (Reference Google images 2013) 7 CONTRAINDICATIONS Bleeding diatheses such as haemophilia A and B and Von Willebrand disease affect blood clotting. Haemophilia A, or Classical Haemophilia, is the most common form, and is due to the deficiency of clotting factor VII (8). Haemophilia B, or Christmas disease, is due to the deficiency of clotting factor IX (9). Haemophilia is rarely seen in females, as it is X-linked. Von Willebrand disease affects 1% of the general population and is transmitted in an autosomal dominant fashion, and affects both clotting factors and platelet function. Children with known clotting diatheses will be referred to WCH to have any ENT surgery carried out in conjunction with a haematologist. Poor anaesthetic risk or uncontrolled medical illness (e.g. diabetes) which can result in intra and post-operative complications. Acute infection. Intraoperative bleeding is greater during acute infection, and there is also the risk of spreading the infection to other structures. Some studies have reported that the risk of bleeding is high following a tonsillectomy where there is a peritonsillar abscess (a “quinsy tonsillectomy” than in an elective tonsillectomy. COMPLICATIONS POSTOPERATIVELY INCLUDE Respiratory compromise. It is also important to keep in mind that in any patient who has upper airway obstruction, removal of that obstruction can lead to post obstructive pulmonary oedema (the sudden loss of negative intrathoracic pressure leads to fluid flowing from capillaries into the lungs). Haemorrhage. Reactionary haemorrhage, which occurs in the first 24 hours and secondary haemorrhage, which occurs after 24hours and up to 10 days later. Pain is the most common complication of the operation. It can also lead to dehydration which results in prolonged hospitalisation. Poor oral intake resulting in dehydration. Injury to lips or teeth is a potential complication of any oral or Oropharyngeal surgery Temporo-mandibular joint subluxation from excessive mouth opening or a weak joint capsule, can lead to severe muscle spasm and inability to open the mouth, until the subluxation is corrected.. Atlanto-axial joint subluxation may be due to patient positioning for Adenotonsillectomy in predisposed individuals (Down’s syndrome, achondroplasia, and rheumatoid arthritis). Newer techniques safeguard against this in such predisposed patients. Grisel’s syndrome is the occurrence of atlantoaxial subluxation in association with inflammation of adjacent soft tissues (usually infection), and is extremely rare. 8 THE PROCEDURE Tonsillectomy is one of the oldest surgical procedures. It was first described by Clesus (first century A.D.) who used a hook to grasp the tonsil then used his finger to incise it. In the 6th century, physicians began to use a knife to remove the tonsil as well as beginning to recognize that being in the correct plane was important for successful outcome. In the 17th century, physicians began to recognize that exposure was important; they recommended having an assistant to hold the patient steady while doing the procedure. As the procedure was painful and difficult for patients to endure further development of “tools” (tonsillotome) enabled the surgeon to grasp and remove the tonsil in one swift move. McKenzie further developed it into the tonsil guillotine. There are many surgical techniques available today including; Cold steel This is the traditional method which involves removal of the tonsils by blunt dissection followed by haemostasis using ligatures. Diathermy This uses electrical energy (alternating current) applied directly to the tissue. It can be bipolar (current passes between the two tips of the forceps) or monopolar (current passes between instrument and a plate attached to the patient’s skin). As current arcs between the instrument tips (bipolar) or instrument and the patient) monopolar), the heat generated may be used to separate and dissect tissues, thus peeling the tonsils away from the pharyngeal wall, and also to promote haemostasis. Diathermy is sometimes used as an adjunct to cold steel surgery to achieve haemostasis. Coblation This involves passing a radiofrequency bipolar electric current through N/Saline. The resulting plasma field of sodium ions c can be used to dissect tissue by disrupting intercellular bonds and causing tissue vaporization. This method generates less heat than diathermy. The Argon plasma coagulator can also be used. This involves a high-voltage monopolar current transmitted to the tissue by a fine jet of ionized Argon gas resulting in the same tissue coagulation or vaporisation MEDICATIONS Paracetamol Pre-operative: □ Oral if documented Intraoperative: □ IV Paracetamol 15mg/kg if not given preoperatively Post-operative: □ Regular Paracetamol 15-20mg/kg 6 hourly 9 Oxycodone Is given post-operatively as a first option for uncontrolled pain at 0.1-0.2mg/kg orally 4 hourly PRN Morphine/Fentanyl Intra-operative □ IV morphine 0.1mg/kg PROCEDURE Preparation for surgery - Usual Preparation for surgery as per Glenelg Community Hospital procedure - Admission to Day Surgery - Most important is inquiry on admission to any recent use of ant-platelet agents such as aspirin and non-steroidal and anti-inflammatory drugs. (NSAIDS). Post operative care Post operative management for ENT patients who have increased potential for airway problems - A nurse may be requested particularly where patients have a history suggestive of obstructive sleep apnoea. These patients must have a nurse present at all times as 1:1 nursing dependency with close monitoring of the patients airway, vital signs and continuous oximetry. Post operative management for ENT patients who do not have an increased risk for airway problems. The patients will be nursed as a ration 1:4 for early and late shifts and 1:5 ratio for night shifts with the usual close monitoring of the patients airway and monitoring of vital signs as well as oximetry as per Clinical Pathway for Adenotonsillectomy Equipment Collect equipment and allocate bed space according to clinical assessment and the need for observation. Airway Monitor closely for early signs of airway obstruction/aspiration especially while patient is still under the effects of sedation or sleeping. 10 Trouble shooting: On arrival to the ward, position the patient on their side to maintain the airway. Do not place a pillow under the head until fully awake and encourage patient to rest in bed until next morning Vital Signs Vital signs are an important component of monitoring the patient’s progress and allows for prompt detection of adverse effects. This constitutes the monitoring of temperature, pulse, respirations and blood pressure (not in children under 12 years of age unless otherwise indicated) as well as oximetry in postoperative patients. Assess and document patient’s status and notify Medical Officer of signs of impaired consciousness. Trouble shooting: A sudden increase in pulse rate does not necessarily mean the child is haemorrhaging it may be they are going to vomit. However, a gradually increasing heart rate is the earliest sign of occult haemorrhage. Pallor also needs to be assessed keeping in mind that some children will be pale after the operation. Hydration Blood and secretions swallowed during the procedure frequently lead to some postoperative nausea and vomiting. Administer IV fluids for the first 24hours or until a satisfactory oral intake resumes. Notify a medical Officer of the amount of vomiting is concerning, or if further intravenous fluids are required to maintain adequate hydration. Trouble shooting: Encourage thin, non-irritant drinks; frozen icy poles often work well. Soft food such as jellies, ice-cream, custard and mashed foods can be helpful but there needs to be some solid food such as toast to encourage gentle removal of the eschar Avoid foods which may irritate or sting the tonsil fossa such as citric juices, salt and vinegar. Encourage small amounts frequently and offer their “favourite” foods. Older children who are finding it difficult to chew can be offered chewing gum to assist in chewing. Good mouth care is required as there can be “bad breath” or “change in taste” following the surgery which can decrease appetite. Encourage the child to brush their teeth and use mouth wash as tolerated. An antiemetic may be administered to alleviate nausea which will assist with eating .DO NOT GIVE AN ANTIEMETIC IF THE CHILD IS HAEMORRHAGING. Pain relief Inadequate pain relief is associated with children’s refusal to eat, which results in dehydration, weight loss and local infection. Aspirin based drugs are not given as pain relief as there is an increased risk of post tonsillectomy haemorrhage. Referred pain can be encountered postoperatively due to inflammation, disruption to oral mucosa, nerve irritation and spam of the exposed pharyngeal muscles. 11 Trouble shooting: Administer regular analgesic especially before meals and at bedtime. Adolescents may need stronger pain relief If Opioids are used in children and adolescents with obstructive sleep apnoea, they must be closely monitored with continuous oximetry Referred pain to the ear or neck is common but watch for signs of trismus or torticollis. Haemorrhage Post operative haemorrhage is the most common serious complication after Adenotonsillectomy surgery. Bleeding can be defined as reactionary haemorrhage or secondary. Complications from a post operative tonsil haemorrhage include; Severe respiratory insult requiring resuscitation (Code Blue) Hypovolemic shock requiring fluid resuscitation and/or blood product Respiratory distress that requires re-positioning to maximize airway support and administration of oxygen to maintain saturation above 95% Primary bleeding occurs intraoperatively. Reactionary bleeding occurs within the first 24 hours postoperatively. A significant primary haemorrhage is treated in the theatre with cautery, ligation or packing in the tonsillar fossa. If any reactionary haemorrhage occurs on the ward, collect the ENT box and notify the ENT Surgeon with the estimated blood loss and vital signs, and call for assistance as necessary. A Nurse must remain in attendance at the bedside at all times. Secondary bleeding can occur after 24 hours up to 14 days with the most frequent time being 6 days post-operatively. If bleeding is not active Monitor and document pulse and respirations and blood pressure ½ hourly with continuous oximetry or as determined by the ENT Surgeon Measure/ estimate all blood vomits. Observe vomit for fresh blood and clots. Do not empty vomit bowls until seen by the ENT surgeon. Document all on fluid balance chart Report immediately to ENT Surgeon any sign of bleeding. If bleeding is active Follow procedure as above Trouble shooting Look for signs of haemorrhage which may include: - excessive swallowing - pallor and sweating - increased pulse rate - excessive blood loss from nose and mouth 12 - excessive fresh blood or clots in any vomits blood seen in the back of the throat, or clots on the tonsil bed Initial signs of post-adenoidectomy bleeding may be controlled using topical nasal decongestants Hydrogen peroxide mouthwash can be effective in settling secondary posttonsillectomy haemorrhage in paediatric patients. It also allows better visibility due to its foaming action removing debris from the tonsillar fossa. if ordered, dilute the peroxide with two parts cold water to make a slightly more palatable mixture encourage older children and adolescents to gargle hydrogen peroxide mouth wash 1% until frothing action occurs and then spit into the r receiver. Do not swallow. The ENT box contains items required to immediately control any post operative bleeding e.g. adenoid, tonsils or epistaxis. It is important to be familiar with the items and their use. Silver Nitrate Sticks-cauterising identified bleeding site DIRECTIONS: The healthcare professional moistens the applicator tip with distilled water and applies it to the affected area. The strength of the action is controlled by the dilution with distilled water. One Grafco® Silver Nitrate applicator is generally sufficient for each application. Cophenylcaine Spray and nozzles □ Local anaesthetic with vasoconstrictor/nasal decongestant Onset of action is rapid and may last for one hour. The Anaesthetic can impair swallowing, so must be used with caution in patients who are bleeding from the pharynx Nasal Drops junior (Otrivin) □ Used in the nose, thus constricts the nasal blood vessels, thereby decongesting the mucosa of the nose and neighbouring regions of the pharynx □ For patients suffering from a stuffy nose to breathe more easily. The effect of Otrivin begins within a few minutes and persists for four to eight hours and sometimes as long as twelve hours. Can also be useful for bleeding from the adenoid bed, and avoids the local anesthetic in Cophenylcaine. 13 Hydrogen Peroxide 3% solution □ May settle minor bleeds by promoting clotting in vessels, and allows better visibility due to its foaming action which cleans the tonsillar fossa 3 Tongue depressors Discharge Prior to discharge ensure the patient meets the following criteria: Stable vital signs Able to ambulate without dizziness Nil signs of haemorrhage Afebrile Tolerating oral intake Discharge education and written information for home management prior to discharge needs to include: Pain management as pain can last up to 10 days and inadequate pain relief is associated with children’s refusal to eat, which results in dehydration, weight loss, and local infection When to call a doctor or return to hospital if signs of bleeding which may be delayed haemorrhage-the most common time being one week post surgery infection limitation of activity can induce bleeding through dislodgement of possible clots Follow up appointment Trouble shooting: It is normal to see white Eschar on the fossa as seen in the illustration above. These are temporary scabs which occur as part of the healing process. They are not a sign of infection and will be replaced with normal mucosa within two weeks of surgery. No attempt should be made to remove them. Often, at around 5-6 days, there is a period of increased pain, which may include pain in the ears, particularly while swallowing. there is often an acceleration of healing response at this time, with- formation of some granulation tissues 14 GLENELG COMMUNITY HOSPITAL Adenotonsillectomy Worksheet Name_____________________________________________RN/EN Date___________________________ Department_____________________ All completed worksheets to be forwarded to the Staff Educator 15 1. Describe how enlarged adenoids and tonsils can alter normal respiratory function. 2. Name 3 indications for an adenoidectomy and 3 for a tonsillectomy 3. What nursing measures would you use to prevent airway obstruction in the immediate postoperative period? 4. You are looking after a three year old patient who has had an Adenotonsillectomy. Identify all of the postoperative observations you are going to do to provide a safe recovery for that child and provide a rationale for each. 16 5. Your four year old patient is refusing to eat or drink. What actions can you take to encourage this child to eat and drink? 6. What would be your actions and where would you access the ENT box in the event of a primary haemorrhage on the ward following an Adenotonsillectomy? 17 7. A five year old child post tonsillectomy is spitting bright blood and saliva, approximately 10-20mls hourly, for the past two hours. Explain what immediate actions you are going to take and why. 8. Henry (15 year old tonsillectomy patient) has eaten half a piece of toast and one cup of cordial. He is complaining it hurts to eat. his mother has come to pick him up. What discharge education are you going to give? Comments: 18 REFERENCES Brown K Morin I, et al Urgent Adenotonsillectomy-An analysis of Risk Factors Associated with Postoperative Respiratory Morbidity, Anaesthesiology 2003; 99; 586-95 Cummings. Otolaryngology: head and Neck Surgery 4th edition 2005 Mosby Inc Does Hydrogen Peroxide Mouthwash Improve the outcome of Secondary PostTonsillectomy Bleed? A 10 year Review, Otolaryngology-head and neck Surgery, Volume 133, Issue 2, August 2005, pages 202-205 Driscolo, C. Darrow D, Kolai PJ Infectious indications for tonsillectomy paediatric Clinics of North America 50 (2003) 445-58 Modbury Hospital Adenotonsillectomy learning Package (S.A. health S.A. Government of South Australia Potter P, Perry A, (2003) Fundamentals of Nursing. The CV Mosby Company, Australia Tabae A, Lin J, Dupiton V, Jones J. The Role of Oral Fluid Intake Following Adenotonsillectomy International Journal Pediatric O2006) 70, (2006) 19