Tonsillitis, Tonsillectomy and Adenoidectomy
advertisement

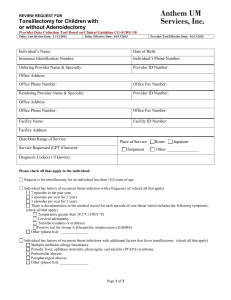
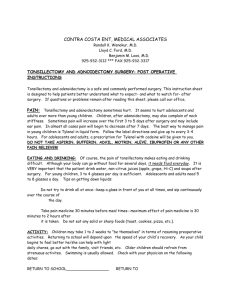
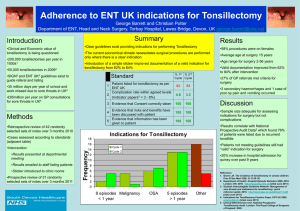
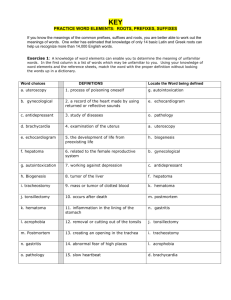
Tonsillitis, Tonsillectomy and Adenoidectomy Steven T. Wright, M.D. Ronald Deskin, M.D. November 5, 2003 Adenotonsillectomy Most commonly performed procedure in the history of surgery $500 million annually in healthcare expenditures History Almost exclusively by Otolaryngologists Celsus in 50 A.D. Caque of Rheims Phillip Syng developed the tonsillotome Anatomy Anatomy Histology Clinical Evaluation Acute Tonsillitis Chronic Tonsillitis Obstructive Tonsillar Hyperplasia Clinical Evaluation Odynophagia, fever, tender cervical lymphadenopathy. Supporting documents, 2 or more Fever> 38.5 Tonsillar Exudate Tender cervical LAD >2cm Positive throat culture Clinical evaluation Viral Lower grade fever Lower WBC, Lymphocytic shift Less tonsillar exudate Bacterial Higher WBC, Granulocytic shift More exudative Recurrent Acute Tonsillitis Seven episodes in a single year Five or more episodes in 2 years Three or more episodes in 3 years Chronic Tonsillitis No true consensus on the definition. Symptoms greater than 4 weeks Differential Diagnosis Infectious Mononucleosis EBV Scarlet Fever Corynebacterium diptheriae Malignancy Complications of Tonsillitis Cervical Adenitis Neck Abscess Peritonsillar abscess Intratonsillar abscess Lemierre’s syndrome Post Streptococcal Glomerulonephritis Joint Pain and oliguric renal failure 10 days after the pharyngitis. Treatment aimed at eliminating the infection and supportive therapy for renal failure. Excellent prognosis in children. Adenoid Hyperplasia Triad Hyponasality Snoring Open mouth breathing Purulent rhinorrhea, post nasal drip, chronic cough, and headache Obstructive Airway Symptoms Snoring Apneic episodes with gasping or choking Daytime hypersomnolence Nocturnal enuresis Behavioral disturbances Heart failure and Failure to thrive Tonsil Size Grade 1 2 3 4 % <25 25-50 51-75 >75 Obstructive Sleep Apnea Polysomnography is the gold standard of diagnosis. Imperative in Adults In children, a convincing history is adequate OSA: RDI > 5, SpO2<90% UARS: RDI <5, SpO2 >90% Primary Snoring: RDI <1, SpO2>90% Medical Therapy TCHP recommends confirming bacterial pharyngitis before beginning antibiotics. Rapid Strep Test Throat Culture Medical Therapy First Line Penicillin/Cephalosporin for 10 days Injectable forms for noncompliance BLPO, co pathogens Macrolides Penicillin allergy Erythromycin/Clarithromycin 10 days Azithromycin (12mg/kg/day) 5 days Medical Therapy Patients with recurrent otitis media history have higher bacterial concentrations with BLPO. Initial treatment with anti-BLP antibiotic. Adenotonsillar size may respond to a one month course of antibiotic therapy. Adenoid hyperplasia may respond to a 6-8 week course of intranasal steroid. Surgical Indications Adenoidectomy Absolute Airway obstruction w/ cor pulmonale Failure to thrive Relative Chronic Nasal Obstruction Recurrent/ Chronic Adenoiditis Recurrent/ Chronic Sinusitis Recurrent acute otitis media/ Recurrent COME Surgical Indications Absolute Obstructive airway with cor pulmonale Severe dysphagia Failure to thrive Relative Recurrent acute tonsillitis Chronic tonsillitis Obstructive Sleep Apnea Peritonsillar Abscess Halitosis Suspected Neoplasia/ Tonsillar hyperplasia Preoperative evaluation Most common lab test is a CBC Coagulation studies when the history or physical examination suggests a bleeding disorder. Lateral Neck/Adenoid films Von Willebrand’s Disease Autosomal dominant bleeding disorder Increased bleeding time and prolonged aPTT. Perioperative management IV Desmopressin (0.3ugm/kg) Serum Sodium Idiopathic Thrombocytopenic Purpura Most common thrombocytopenia of childhood. 90% resolution by 9-12 months Splenectomy IVIG preoperatively Innovative Surgical Techniques Cold Dissection Electrosurgery Intracapsular partial tonsillectomy Harmonic Scalpel Radiofrequency tonsillar ablation and coblation. Electrosurgery Most popular technique for tonsillectomy Equivalent or superior to the other methods of tonsillectomy. Intracapsular Partial Tonsillectomy 45 degree Microdebrider (1500rpm). Advantages As effective as standard tonsillectomy in relieving obstruction. Less pain, quicker return to normal diet Disadvantages: Tonsillar regrowth Greater intraoperative blood loss Harmonic Scalpel Advantages: Better visibility Smaller risk of stray energy shocks Improved post operative pain Disadvantages: Must use alternate device for adenoidectomy Similar intraoperative blood loss. Radiofrequency tonsillar coblation Coblation is superior to ablation. Early elimination of pain and reduced pain medicine usage. Early resumption of normal diet. Currently inadequate for adenoidectomy Adjuvant Therapies Perioperative local anesthetic 0.25% bupivicaine w/ 1:100,000 Epinephrine Advantages: ease of dissection, postoperative pain Disadvantages: Airway obstruction, cardiac dysrrhythmias, seizures Adjuvant Therapies Perioperative antibiotics Fewer episodes of fever, offensive odor, improved oral intake, less pain, fewer days to return to normal activity Cardiac abnormality Adjuvant Therapies Perioperative Steroids Dexamethasone (0.15-1.0mg/kg) Two times less likely to have an episode of postoperative emesis, and more likely to advance to eating a soft diet. Reducing postoperative pulmonary distress, subglottic edema, pain reduction. Adjuvant Therapies Pain control Tylenol and Tylenol w/ codeine are the most commonly used. Similar pain control, less oral intake with codeine versus Tylenol alone. NSAIDS still controversial. Complications Mortality rate is 1 in 16000-35000. Anesthetic complications Eustachian tube injury VPI Nasopharyngeal stenosis Pulmonary Edema Atlantoaxial subluxation 23 hour observation Age younger than 3. Obstructive sleep apnea/craniofacial syndromes involving the airway. Systemic disorders Poor socioeconomic situation Peritonsillar abscess Emesis or Hemorrhage Post Operative Hemorrhage The best treatment is prevention. Early vs. Delayed hemorrhage. Overnight observation and venous access Surgical intervention. Carotid angiography if any suspicion of carotid artery injury. Case Study 8yo male referred to the Pediatric clinic for evaluation and treatment of recurrent tonsillitis. History Only 2 episodes of documented pharyngitis in the past 12 months, strep negative, only missed 5 days of school total last year. Loud snoring, frequent pauses up to 5 seconds terminated with gasps of breath. Physical Examination Normal facies, open mouth breathing, tonsils 3+, no cleft deformities. Remainder of exam is normal. Case Study Undergoes uneventful tonsillectomy and adenoidectomy with 23 hour observation. On follow up visit 2 weeks postoperatively, his mom complains that he doesn’t like some of his favorite foods. He says they taste “yucky”. Decreased perception of taste with no smell abnormalities. Diagnosis Dysgeusia Unknown mechanism- thought to be due to prolonged pressure on the tongue by the mouth retractor. Treatment is reassurance. Bibliography Allen GC, et al. “Adenotonsillectomy in Children with von Willebrand Disease.” Archives of Otolaryngology 1999, May; 125(5) pp547-551. Bailey BJ: Head and Neck Surgery- Otolaryngology, 3rd ed. Philadelphia, Lippincott-Raven, 2001, pp 979- 1006. Brook I, et al. “Microbiology of Healthy and Diseased Adenoids.” Laryngoscope 2000, June; 110(6): pp994-999. Darrow D, Siemens C. “Indications for Tonsillectomy and Adenoidectomy.” Laryngoscope 2002, August; 112(8 part 2): pp6-10. Derkay C, Maddern B. “Innovative Techniques for Adenotonsillar Surgery in Children: Introduction and Commentary.” Laryngoscope 2002, August; 112(8 part 2): p2. Friedman M, et al. “Radiofrequency Tonsil Reduction: Safety, Morbidity, and Efficacy.” Laryngoscope 2003, May; 113(5): pp882-887. Goldstein N. “Child Behavior and Quality of Life Before and After Tonsillectomy and Adenoidectomy.” Archives of Otolaryngology 2002, July; 128(7): pp770-775. Harley E. “Asymmetric Tonsil Size in Children.” Archives of Otolaryngology 2002, July; 128(7): pp767-769. Johnson L, et al. “Complications of Adenotonsillectomy.” Laryngoscope 2002, August; 112: pp35-36. Kay D, et al. “Perioperative Adenotonsillectomy Management in Children: Current practices.” Laryngoscope 2003, April: 113(4): pp 592-597. Koempel J. “On the Origin of Tonsillectomy and the Dissection Method.” Laryngoscope 2002, September; 112(9): pp1583-1586. Koltai P, et al. “Intracapsular Partial Tonsillectomy for Tonsillar Hypertrophy in Children.” Laryngoscope 2002, August; 112 (8 part 2): pp 17-19. Leinbach R, et al. “Hot versus Cold Tonsillectomy: A systematic review of the literature.” Otolaryngology-Head and Neck Surgery 2003, October; 129 (4): pp360-364. Maddern B. “Electrosurgery for tonsillectomy.” Laryngoscope 2002, August; 112(8 part 2): pp11-13. Mui S, et al. “Efficacy of Tonsillectomy for Recurrent Throat Infection in Adults.” Laryngoscope 1998, September; 108(9): pp1325-1328. Plant R. “Radiofrequency Treatment of Tonsillar Hypertrophy.” Laryngoscope 2002, August; 112(8 part 2): pp20-22. Steward D, et al. “Do Steroids Reduce Morbidity of Tonsillectomy? A Meta-analysis of Randomized Trials.” Laryngoscope 2001, October; 111(10): pp1712-1718. Stewart R, et al. “Dexamethasone reduces pain after tonsillectomy in adults.” Clinical Otolaryngology and Allied Sciences 2002, October; 27(5): pp321-326. Thomsen J, Gower V. “Adjuvant Therapies in Children Undergoing Adenotonsillectomy.” Laryngoscope 2002, August; 112(8 part 2): pp32-34. Warltier et al. “Effects of Non-Steroidal, Anti-inflammatory Drugs on Bleeding Risk after Tonsillectomy, Meta-analysis of Randomized Controlled Trails.” Anesthesiology 2003, June; 98(6): pp1497-1502. Wiatrak B, Willging J. “Harmonic Scalpel for Tonsillectomy.” Laryngoscope 2002, August; 112(8 part 2): pp14-16. Younis R, Lazar R. “History and Current Practice of Tonsillectomy.” Laryngoscope 2002, August; 112 (8 part 2): pp3-5.