Diarrhea & Constipation: Pathophysiology, Diagnosis, & Management
advertisement

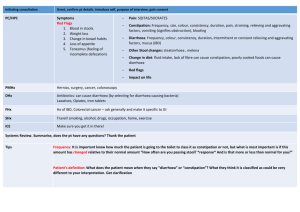
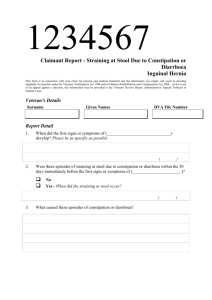
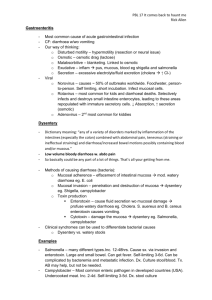
Objective 6. Discuss the pathophysiology, symptoms, d/dx and investigations of diarrhoea and constipation. Diarrhoea is the passage of >250g of liquid stool per day, it can be a sign of infection, malabsorption or osmotic and secretory diarrhoea, if it is bloody it may be a sign of infarction or dysentery (bloody with mucous stool, sign of infection). It can also occur in the small and large bowel. Diarrhoea can be caused by: mucosal atrophy in the small intestine with loss of the villi and concurrent loss of the brush border disaccharidases. Problems with cell mediated immunity which predispose patients to parasitic infection of the bowel. Loss of lactase, a disaccharidase, which causes problems when dairy products are consumed. Types of diarrheal diseases: 1. Acute (<3 weeks) 2. Chronic (>4 weeks) These are further subdivided into: Invasive Osmotic- excessive amounts of solutes retained in the intestinal lumen, as water is not absorbed, diarrhoea will result. Osmotic diarrhoea is usually as a result of ingestion of poorly absorbed substrates for e.g. carbohydrate or divalent ions such as mannitol or sorbitol, Epson salt MgSo4 and some antacids MgOH2 and malabsorption, commonly carbs such as lactose. Osmotic diarrhoea stops if the patient stops consuming the poorly absorbed solute or fasts for a certain period. Secretory- caused when secretion of water into the intestinal lumen exceeds absorption. Will not resolve after a 2-3 day fast. Malabsorption Test used to diagnose diarrheal diseases: a) Faecal smear for leucocytes (invasive diarrhoea) b) Calculation of stool osmotic gap (SOG) [2 * (random stool Na++ random stool K+}, where 300mOsm/kg = normal plasma osmolality levels, osmotic gap < 50mOsm/kg = secretory diarrhoea (characterised by a loss of isotonic fluid e.g. on cholera) indicating that the diarrheal fluid POsm approximates the normal POsm and an osmotic gap > 100 mOsm/kg = osmotic diarrhoea (e.g. in lactase deficiency (a common genetic defect in Native Americans, Asians, and Africans. Colonic anaerobes degrade undigested lactose into lactic acid and H2 gas leading to abdominal distention with explosive diarrhoea), or due to certain laxatives) indicating a hypotonic loss of stool caused by the presence of osmotically active substances. Malabsorption: this is chronic diarrhoea with increased faecal excretions of fat (steatorrhea). Concurrent deficiencies of fat- soluble vitamins, minerals, carbohydrates and proteins are commonly present. Diarrhoea associated with deranged motility. Disorder in motility can accelerate the transit time and decrease the absorption of water and nutrients resulting in diarrhoea even of the absorptive process was proceeding properly. Constipation This is a symptom generally defined as when bowel movements occur three or fewer times a week and are difficult to pass. It is due to reduced colonic motility and can be caused by a lack of fibre intake, immobility drugs that reduce transit time (antidepressants, antacids with Aluminium or Calcium, antihistamines, diuretics and anti -Parkinson drugs) and depression. It is also associated with small bowel disease and presents as colicky pain (which is a sharp localised gastrointestinal or urinary pain that can arise abruptly and tends to come and go in spasm like waves) accompanied by constipation and the inability to pass gas. If left unrecognized, it can develop into sequelae such as anorectal disorders. If a patient experiences at least two of the following symptom over a 6 month period, it can be deemed constipation: fewer than three spontaneous bowel movements per week Straining for more than 25% of defecation attempts Lumpy or hard stools for at least 25% of defecation attempts Sensation of anorectal obstruction or blockage for at least 25% of defecation attempts Sensation of incomplete defecation for at least 25% of defecation attempts Manual maneuvering required to defecate for at least 25% of defecation attempts Also the patient must rarely have loose stools present without use of a laxative and must not meet Rome IV criteria for IBS. Other symptoms of constipation are: Abdominal bloating Pain on defecation Rectal bleeding Spurious diarrhoea Low back pain Feeling of incomplete evacuation Digital extraction Tenesmus Enema retention The following signs and symptoms, if present, are grounds for particular concern: Rectal bleeding Abdominal pain (suggestive of possible IBS with constipation [IBS-C]) Inability to pass flatus Vomiting Constipation is diagnosed by: Rectal and perineal examination Imaging studies to rule out process that may cause colonic ileus, sources of sepsis or intraabdominal problems in patients with leucocytosis or other systemic intra-abdominal processes, or to determine the cause of chronic constipation. Lower GI endoscopy, colonic transit study, defecography, anorectal manometry, surface anal EMG and balloon expulsion testing. Management Initially treatment may be manual disimpaction and transrectal enemas Dietary changes (increase fibre and fluid intake and decreased ,milk products, coffee, tea, alcohol)and exercise rather than laxatives, enemas and suppositories. Bulk forming medications e.g. psyllium Emollient stool softeners e.g. docusate Rapidly acting lubricants e.g. mineral oil Prokinetics e.g. tegaserod Stimulant laxatives e.g. senna Prucalopride Lubiprostone Linaclotide Mu opioid receptor antagonists. Constipation may originate from within the colon and rectum or externally via the following processes: Colon obstruction Slow colonic motility Outlet obstruction (anatomical or functional) Anatomic outlet obstruction may derive from intussusception of the anterior wall of the rectum on straining, rectal prolapse, and rectocele; functional outlet obstruction may derive from puborectalis or external sphincter spasm when bearing down, short-segment Hirschsprung disease, and damage to the pudendal nerve, typically related to chronic straining or vaginal delivery Hirschsprung disease in children Chagas disease