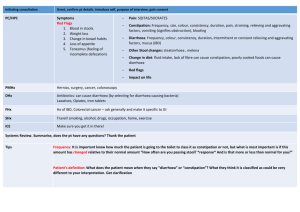
Classification of Diarrhoea
advertisement
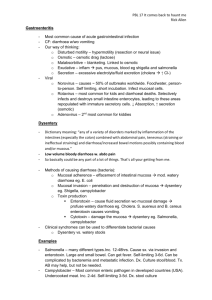
[PBL PATIENT CASE 10] Diarrhoea Classification of Diarrhoea Secretory (non invasive): Decreased absorption and increased intestinal secretion into the lumen result in watery diarrhoea. Organisms which produce diarrhoea by production of toxin(s) produce watery diarrhoea, and usually involve the small intestine. Vibrio cholera (Cholera) and enterotoxigenic E .coli are most common but can also occur due to actions of hormones, presence of bile salts/fatty acids in the colon following ileal resection and some laxatives. In watery diarrhoea usually there is loss of lots of fluid and electrolytes from the body which results in dehydration. Cholera toxin binds to receptor on small intestine which increases cAMP and causes Cl- secretion. Water follows into lumen. Additionally, Na and Cl absorption are inhibited. Invasive: Those organisms which invade the gut mucosa usually produce bloody diarrhoea (dysentery), produce an inflammatory response and primarily affect the large bowel. Shigella and E.histolytica are the prototype organisms. In contrast to secretory diarrhoea, invasive diarrhoea results in much less fluid and electrolytes lost in the stool. Therefore, dehydration is not a major feature. Inflammatory: Not really sure how this is different to Invasive??? Most sources classified inflammatory as invasive as it also involves mucosal damage and loss of blood in stools. Only difference of note is the inclusion of chronic inflammatory conditions such as ulcerative colitis and Crohn’s which produce bloody diarrhoea in response to inflammation. Osmotic: Due to generalised malabsorption, specific defect in absorption or patient ingested a nonabsorptive substance (eg. purgative such as magnesium sulphate). High concentrations of solute remain in the lumen of the colon, and the gut mucosa acts as a semi-permeable membrane so that fluid enters the bowel by osmosis due to the hypertonicity of the lumen. Diarrhoea stops when patient is fasting/stops eating the substance that isn’t absorbed. Abnormal Motility: Diabetic, removal of vagus nerve, or hyperthyroidism. Abnormal motility of upper GIT so that frequency of defecation is high although volume is not – therefore not really true diarrhoea.