L3-Host-Defense
advertisement

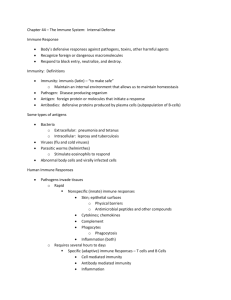
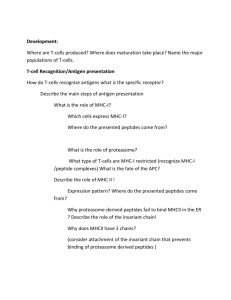
Lecture 22: Immune Systems How do hosts ameliorate the ever-present threat of parasites? I. Prophylactic behavior – individual behavior that reduces parasite risk and transmission A. Spatial avoidance B. Temporal avoidance C. Migration D. Prey Avoidance E. Individual avoidance F. Selfish herd G. Anticipatory Defenses II. Social Immunity – group behavior that reduces parasite risk and transmission A. Allogrooming B. Social Exclusion C. Removing infected / dead individuals III. Immune system – collection of mechanisms providing defense against parasites, pathogens and abnormal cells. Categorized into either innate or adaptive systems. Innate immunity –Rapid response. General (as opposed to specific) response against broad classes of pathogens (e.g. fungi, gram-negative bacteria, gram-positive bacteria, etc). Exists in all plants and animals; evolutionarily ancient. A. Barrier defense – first line of defense 1. Skin / exoskeleton 2. Mucosal membrane – traps pathogens and removes (e.g. sneezing / coughing) 3. Antibacterial secretions – secretions found in multiple sites (saliva, mucous, gut, metapleural gland in ants) that are non-specific antibacterial agents (e.g. lysozymes) B. Internal Defenses – second line of defense when barrier defenses fail. 1. Phagocytic cells – pseudopods engulf and transport invaders into lysosome, where it is killed and digested. Some phagocytes also ‘present’ pieces of invader to other cells. a. vertebrate phagocytes 1. macrophages –most common. Found throughout body 2. neutrophils – very common. Found in blood. 3. dendritic cells – found in tissues that contact environment. antigen presenting cell 4. eosinophil – minor phagocyte b. Toll (invertebrates) and Toll-like receptors (TLRs; vertebrates) are intramembrane and intracellular proteins that recognize pathogen motifs. These are highly conserved across animal species. 2. Antimicrobial peptides (AMPs) – activation of Toll may result in production of antimicrobial peptides (small molecules aimed at specific classes of pathogens) 3. Inflammation – Changes brought about by signaling molecules released upon injury or infection (vertebrates only). Histamine increases blood vessel permeability brining phagocytes and AMPs to site of injury. Lecture 22: Immune Systems 4. Natural Killer cells (NK) – vertebrates only. Detect and destroy infected and cancerous cells by inducing cell apoptosis (programed cell death). Does not phagocytize. 5. antivirals a. interferons – molecules released by infected cell to warn neighboring cells of threat. Neighbors halt protein production, stopping viral transmission. b. RNA interference (RNAi) – enzymes dice-up viral messenger RNA (mRNA) before it creates viral proteins. Aimed at specific mRNAs. Major Plant defense Adaptive (acquired) immunity A. Adaptive immunity responds to pathogens with tremendous specificity. Remembers past infections for quicker response (two words: specific and memory). 1. Cell-mediated immunity – comprised of helper T-cells and cytotoxic T-cells. Helper Tcells coordinate adaptive immune response. Cytotoxic T-cells defend against intracellular pathogens and cancer. 2. Humoral immunity – comprised of B-cells, which defend against extracellular Pathogens B. T and B cell structure 1. Each cell studded with 1000’s of antigen receptors; each cell can recognize only one antigen. However, there are millions of different B and T cells. 2. Antigen is a substance the elicits an immune response C. Helper T-cells - Coordinate adaptive immune response by activating B and cytotoxic T-cells Step 1 – Antigen presenting cell (e.g. dendritic cell, macrophage or B-cell) engulfs a Pathogen Step 2 – antigen fragment presented MHC (major histocompatibility complex) molecule Step 3 – Helper T-cell binds to MCH and antigen. This stimulates cytokine release from both the helper T-cell and antigen presenting cell. Cytokines signal T-cell to divide (cytokines – signaling molecules used for communication) Step 4 – Cytokines recruit B-cells and cytotoxic T-cells to scene, which then effect the immune defense. D. B-cells Step 1 – B-cell encounters pathogen and internalizes antigen Step 2 – antigen presented via MCH Step 3 – Helper T-cell binds B-cell, releases cytokines that induce B-cell to divide into memory cells (for future infection) and plasma cells (for current infection) Step 4 – plasma cells secrete antibodies (antibodies are soluble antigen receptors also known as immunoglobulins) E. Antibodies 1. can defend against a pathogen via a. viral neutralization – block ability to enter host cell b. opsonization – facilitates phagocytosis c. activation of complement system – induces cell lysis F. Cytotoxic T-cells 1. Bind to MHC presented antigens from infected / cancerous cells and induce apoptosis (cell death) G. Immunological Memory 1. Previous exposure produces memory cells, which greatly shortens the time it takes to mount a response. Lecture 22: Immune Systems III. Lymphatic system A. Crucial to immunity 1. Lymphatic vessel – network of vessels throughout the body. Interstitial fluid (fluid between cells) containing pathogens or cellular debris drain into the vessels. 2. Lymph nodes – lymph collects in nodes that are packed with immune cells 3. Spleen – although not directly connected to the lymph system, the spleen filters blood, removes opsonized pathogens and synthesizes antibodies. It is similar to a giant lymph node.