CHF Drugs: Pharmacology Study Guide for Heart Failure Treatment
advertisement

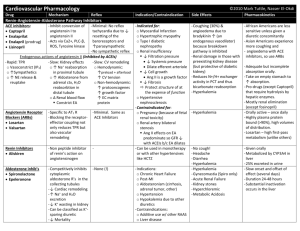
CHF Drugs CHF: Cardiac output at the expense of intravascular volume overload. Activation of SNS and Renin-Angiotensin System produces: Norepinephrine, Angiotensin II, ADH (Vasopressin), Aldosterone Norepinephrine, Angiotensin II, and ADH are part of neurohormone storm. They produce increase in TPR = increase in afterload = decrease in CO. Renal Vascular resistance = GFR CO = Renal blood flow + GFR Therefore, patient w/ decompensated heart failure is characterized as a patient with decreased CO at the expense of increased TPR and intravascular volume overload. Purpose of Pharm Therapy: decrease TPR and afterload, and increase CO, Renal blood flow, and urine output. Drug MOA / Pharmacodynamics Furosemide (Lasix): dose 20 mg/day - >400 mg/day Bumetanide: shorter acting, better GI absorption (same w/ Toresmide) Thiazide: Metolazone HCTZ Don’t reduce mortality, just help symptoms! Angiotensin Converting Enzyme Inhibitors (ACE Inhibitors) Enalapril (2x/day) Lisinopril (1x/day) REDUCE MORTALITY SE / Contraindications Acts at loop of henle to prevent sodium reabsorption and thus increasing urine production Loop Diuretics Furosemide (40mg) Bumetadine (1mg) Toresmide (10-20mg) ACE Inhibitor: Inhibits angiotensin-converting enzyme to prevent angiotensin II (a vasoconstrictor) production. Thus, ACE inhibitors cause angiotensin I levels to increase. Preventing reabsorption of sodium leads to increase Na load in distal convoluted tubule – you start to increase avidity to Na (basis of Lasix resistance). Therefore, you increase dose and add a thiazide (inhibits sodium reabsorption in distal convoluted tubule). -Levels of bradykinin increase which contributes to decrease in TPR and vasodilation. -Angiotensin II typically stimulates hypothalamus to drive thirst mechanism and stimulates posterior pituitary to generate ADH in addition to adrenal gland stimulation of aldosterone. Therefore, ACE-I will: - products of the Neurohormone l Storm - Cardiac Output - symptoms of Heart Failure - Survival - vascular activation, atherosclerosis progression, and thrombosis - fibrinolysis Wide & safe dosing: 2.5-40 mg/day Orally active & well absorbed High doses of furosemide ototoxicity Sulfur allergy!!! (Only ethacrynic acid is sulfur free). Associated w/ arrhythmias due to K and Mag wasting. SE: Hypovolemia, Hypokalemia, Hypotension, Renal Failure, Alkalosis SE of Thiazide: hypokalemia Bradykinin is responsible for the SE profile - chronic hacking dry cough - hyperkalemia - angioneurotic edema (class specific to if you get it on one ACE inhibitor, you’ll get it with all. SE profile occurs in 20 % of all patients. Considerations: Class III & IV HF hypotension if not monitored properly, which will decrease renal function and injure kidneys more. Over time, you may get ACE escape (so then you start to use ARBs) Drug MOA Pharmacodynamics SE / Contraindications AT Receptor Antagonists Losartan Valsartan Angiotensin Receptor Blockers (ARBs): direct blockage of AT 1 receptor, which is responsible for vasoconstriction, ADH, and aldosterone release. By blocking AT-1, we would block effects of angiotensin II on receptor, therefore decreasing TPR, decrease aldosterone, and improve patients. Don’t use WITH ACE-I: combination may increase risk of renal failure and hyper REDUCE MORTALITY Beta-Blockers Carvedilol (B1/B2) Metoprolol (B1) Bisoprolol (B1) Bind tightly to beta receptor blocking the effects of Norepinephrine in the mediator of SNS. REDUCE MORTALITY Need to monitor K+ and serum Cr! -No increase in bradykinin. -Best used in ACE intolerant (cough) -Orally active: once a day, dose needs to be titrated -Losartan – just not as effective as ACE inhibitors CV Effects of Beta-Blockers in CHF Patients - HR = tachycardia of Heart Failure (Important in patients with Coronary Artery Disease = Myocardial Oxygen Consumption) - Total Peripheral Resistance = Myocardial Afterload - A-V nodal conduction = (able to slow the ventricular response rate in Atrial fibrillation) - Combined ACE-I & BB in RCTs demonstrate Survival -Bronchospasm -Slowing of AV conduction (heart block) -Hypotension -Depression (esp in elderly) -Impotence can limit use in young males Metropolol: 12.5 mg – 100 mg (extended release daily & 2x/day) - Goal dose is 200 mg Carvedilol: 3.125 mg – 25 mg twice a day Aldosterone Inhibitors Spironolactone Eplerenone REDUCE MORTALITY ADH Inhibitors Hydralazine and Nitrates REDUCE MORTALITY Direct inhibition of the mineralocorticoid, Aldosterone, thereby inhibiting SodiumPotassium exchange in the kidney and preventing the excretion of potassium Prevents aldosterone, which normally activates fibroblasts and lays out more scar tissue. Commonly called potassium sparing diuretics, but in actuality they’re weak diuretics Oral – 12.5 – 50 mg/day Drugs in combination w/ ACE-I and B-blockers in patients w/ dilated cardiomyopathy improve symptoms and reduce mortality by decreasing myocardial fibrosis. Hyperkalemia is a direct effect of the drug, risk factors: Age > 70, Decreasing Renal Function: Cr > 2.3 mg%, Inability to monitor potassium Spironolactone: produces a 20 % incidence of gynecomastia in the male Eplerenone: No estrogenic stimulation but a weaker aldosterone antagonist Need to monitor K+ and serum Cr! ACE-I just reduces death from HF, but beta blockers and aldosterone antagonists reduce sudden death (theory is you decrease scarring in heart so less chance of arrhythmias). ADH inhibitors are available but only for correction of hyponatremia They have NO beneficial effect on either morbidity or mortality in heart failure patients over and above ACE Inhibitors, Beta-Blockers, and Aldosterone Inhibitors Vasodilators! Vasoconstriction is bad especially if you have a myopathic heart because increase in afterload (blood pressure in this case) will decrease stroke volume. With a myopathic heart, you’ll have a greater reduction of SV. Therefore, use vasodilators to decrease afterload. Mean dose – 3.8 tablets a day (1 tablet = 37.5 mg hydralazine/20 mg nitrates) Acute Decompensated Heart Failure Tx Drug IV Diuretics Oxygen MOA Treatments and Pharmacodynamics SE / Contraindications - Pts w/ significant fluid overload should be treated promptly. - If pts are receiving too much, the initial IV dose should equal or exceed their chronic daily dose. - Urine output and signs/symptoms of congestion should be serially assessed and dose adjusted accordingly to relieve symptoms, reduce volume excess, and avoid hypotension. Previously not on diuretics: Furosemide 20-40 mg IV and then titrate. Adequate response within 2 hrs. – double the dose. Pts w/ renal dysfunction may need larger dose. Already on chronic diuretics: double the oral dose. Continuous dosing: furosemide drip at 10 mg/hr 240 mg/IV daily Additionally, may use thiazide diuretics, ultrafiltration, hemodialysis, or augment CO to improve renal function. Titrate to keep patient comfortable – keep oxygen sat > 90 % Non-invasive ventilation: - CPAP or Bopp - Provides positive end-expiratory pressure - Used in pts w/ respiratory distress (pulm edema), respiratory acidosis, persistent hypoxia - Improves oxygenation - Decreases need for mechanical ventilation Vasodilators (IV) - Use if urgent need for afterload reduction or refractory heart failure and low CO. Adjunct to diuretic therapy! - Reduce LV filling pressure, acts as venodilator Nitroglycerin - High doses can decrease systemic vascular resistance (afterload) (nitrate) - IV medication – can titrate quickly Nitroprusside (nitrate) Nesiritide (natriuretic peptide) - preferred agent - balanced vasodilator and venodilator - decreases LV filling pressure AND decreases systemic vascular resistance (afterload) - afterload reduction improves LV Stroke Work - balanced vasodilator and venodilator - decreases LV filling pressure AND decreases systemic vascular resistance (afterload - promotes natriuretic - use w/ pts w/o hypotension or cardiogenic shock or who are symptomatic despite therapy hypotension, headache hypotension, metabolism produces cyanide which can limit use hypotension and risk of worsening renal function Inotropes (IV) - Bridge therapy for end stage HF patients who are awaiting definitive therapy or surgery (transplant, LVAD, etc) - Inotropes can improve symptoms but does not improve mortality. Increases atrial and ventricular arrhythmias. PDE (-) - Increases inotropy by inhibiting breakdown of cAMP Milrinone - Reduce systemic and pulmonic vascular resistance - Improve LV diastolic compliance - Increases CO, Decreases afterload, decrease filling pressures B1 receptor - Increases SV and CO Dobutamine agonist - Modest decrease in systemic vascular resistance and filling pressures Hypotension