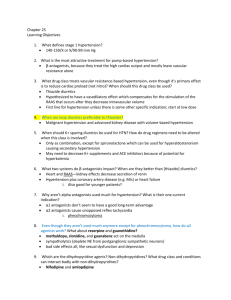
Cardiology Review: HTN
advertisement

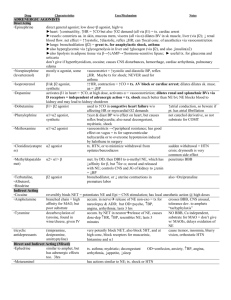
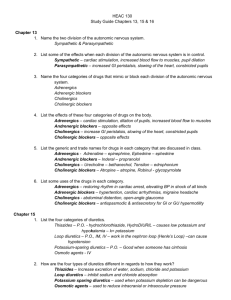
Cardiology Review: HTN Julia Akaah M.D. Of the estimated 50 million Americans that have HTN (average BP>140/90): 90% have essential HTN Remainder have secondary HTN Renal parenchymal disease Renovascular disease Pheochromocytoma Cushing’s syndrome Primary hyperaldosteronism Coarctation of the aorta Autosomal dominant or recessive diseases of the adrenal-renal axis that result in salt retention Laboratory Evaluation Help identify patient’s baseline and any evidence of organ damage Urinalysis Hematocrit Electrolytes, BUN, Cr, glucose, Ca Uric acid Fasting lipid profile CXR ECG echocardiogram Initial Management Goal of treatment is to prevent long term sequelae Most patients should be given a 3-6 month opportunity to reduce BP by nonpharmacologic means Pharmacologic therapy Diuretics Beta Blockers Alpha1-receptor blockers Centrally acting Adrenergic Antagonists Calcium channel blockers ACE-I/ARBs Vasodilators Diuretics: Mechanism of Action Initiate natriuresis and decrease intravascular volume May initially increase peripheral resistance and decrease cardiac output May produce mild vasodilation by inhibiting Na entry into vascular smooth muscle cells Thiazide diuretics HCTZ, chlorthalidone, metolazone Block sodium reabsorption in distal convoluted tubule by inhibition of the thiazide sensitive Na/Cl co transporter Usually ineffective when creatinine >2.0mg/dl Side effects: Weakness ms. Cramps Impotence Hypokalemia Hypomagnesemia increased LDL and TG Hypercalcemia Hyperglycemia Hyperuricemia Hyponatremia thiazide induced pancreatitis Loop diuretics furosemide, torsemide, bumetanide Block Na reabsorption in the thick ascending loop of Henle by inhibiting the Na/K/2Cl cotransporter Most effective in patients with associated renal insufficiency Can cause hypomagnesemia, hypocalcemia, hypokalemia, increase fasting glucose, postural hypotension and reversible ototoxicity (dose related) Potassium sparing diuretics spironolactone, amiloride, triamterene Spironolactone competitively inhibits the action of aldosterone Triamterene and amiloride inhibit the reabsorption of Na and secretion of K Weak agents when used alone therefore combined with thiazide for added potency Hyperkalemia, gynecomastia, renal tubular damage and renal calculi with combination of triamterene and HCTZ Beta Blockers Competitive inhibition of catecholamines at B- adrenergic receptors which decreases heart rate, cardiac output, and decreases plasma renin Advantageous in patients with increased adrenergic drive, LVH and previous MI and stable HF Cardioselective beta blockers have primarily beta-1 blocking effects (atenolol, metoprolol, bisoprolol, etc.) therefore can be given at low doses, with caution in mild COPD, DM and peripheral vascular disease At higher doses, selectivity is lost Nonselective (nadolol, propranolol, timolol) Alpha and beta antagonists (labetolol, carvedilol) As lipid solubility increases, the liver metabolizes more of the drug and more enters the brain, and therefore duration of action is shorter As lipid solubility decreases the drug is renally eliminated and less drug enters the brain and therefore duration of action is longer Very lipid soluble: propranolol, metoprolol, timolol Least-lipid soluble: atenolol, betaxolol, nadolol Side effects: high degree AV block, HF, Raynauds, impotence, insomnia, depression, contraindicated in asthma, severe COPD, and DM Alpha1-receptor blockers prazosin, terazosin, doxazosin Block alpha receptors, producing arterial and venous vasodilation Side effects First dose effect Hypotension Syncope May decrease total cholesterol and TG levels and increase HDL Centrally acting Adrenergic Antagonists methyldopa, clonidine Stimulate presynaptic alpha 2-adrenergic receptors leading to decrease in peripheral sympathetic tone and systemic vascular resistance Side effects: bradycardia, drowsiness, dry mouth, orthostatic hypotension, galactorrhea and sexual dysfunction acute withdrawal of clonidine can cause rebound HTN Calcium channel antagonists Effective in both blacks and whites Dihydropyridines (nifedipine, felodipine, amlodipine etc.) Nondihydropyridines (verapamil, diltiazem) Cause arteriolar vasodilation by selective blockade of the slow inward calcium channels in vascular smooth muscle cells. May cause initial natriureses Side effects: constipation, nausea, HA, orthostatic hypotension, lower extremity edema Inhibitors of the renin-angiotensin system: ACE-I Inhibition of ACE leads to arteriolar and venous vasodilation and to natriuresis beneficial in pts. with associated heart failure or kidney disease Retard progression of nephropathy and proteinuria ACE-I prevent recurrent MI and the development of CHF in persons who have had an MI complicated by reduced LV function Dose reduction in renal insufficiency and contraindicated in pregnancy Side effects: orthostatic hypotension, hyperkalemia, cough, angioedema, and loss of renal function Angiotensin II receptor blockers losartan, valsartan, candesartan Cause decreased peripheral resistance by by inhibiting the actions of angiotensin II at its cell surface receptor Side effect profile similar to ACE-I but decreased likelihood of cough Avoid in pregnancy Vasodilators hydralazine, minoxidil Direct dilatation of arterioles Dose should not exceed 200mg/d because of the increased risk of lupus like syndrome Side effects: headache, palpitations, tachycardia, fluid retention, lupus like syndrome, and peripheral neuropathy with hydralazine Side effects: weight gain, hirsutism and pericardial effusions with minoxidil Don’t use in ischemic heart disease, dissecting aneurysm, or cerebral hemorrhage because it can increase cardiac output and cerebral blood flow Drugs for monotherapy: diuretics, B blockers, CCBs, ACEI, alpha-beta blockers, and ARBs Diuretics and calcium antagonists are more effective in blacks and elderly Centrally acting alpha agonists are not used as monotherapy but are appropriate in combination with diuretics Vasodilators are best used as third drug in combination with diuretics and adrenergic inhibitors Hypertensive crisis Hypertensive Urgency DBP >120-130mmHg BP reduction within several hours Hypertensive Emergency SBP >210, DBP >130 Manifestations of acute organ disease Immediate BP reduction by 20-25% Inservice topics related to HTN: Antihypertensive monotherapy for elderly black patient Rebound hypertension with clonidine Identify drugs that can unmask hyporeninemic hypoaldosteronism Hypertension in DM with proteinuria Hypertensive crisis In several office visits, a 33 yr old woman has an average BP of 150/105 mmHg. She has a strong family history of HTN. She is asymptomatic. Except for mild obesity, the physical examination is normal. The results of routine laboratory studies are also normal. She is a nonsmoker. She states that she recently married and is trying to get pregnant. In addition to lifestyle recommendations, what is the most appropriate drug to consider for BP reduction? a. Atenolol b. Methyldopa c. Lisinopril d. HCTZ e. Losartan