fitz_exam_3_objectives
advertisement

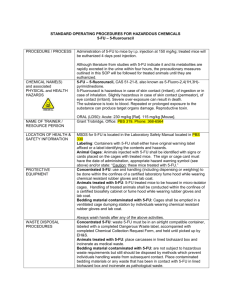
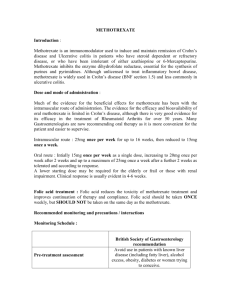
Exam 3: Fitzakerley’s Learning Objectives Anti-neoplastics I: General Concepts: 1. List the targets and mechanisms of action of antineoplastic drugs. Be able to rank these with respect to specificity and be able to predict side effects based on the types of cells that are targeted by cytotoxic agents. a. Processes targeted (from least to most specific) i. Rapid cell growth (cytotoxic drugs) ii. Angiogenesis/metastasis iii. Lack of differentiation iv. Cell surface markers / lack of immune response v. Defective gene products b. Cells affected by cytotoxic drugs: i. Cancer cells ii. Bone marrow (= most common doselimiting complication) iii. GI mucosa (N/V) iv. Hair follicles (alopecia) v. “Radiation recall rxn” – erythema & desquamation of skin at site of prior rad Tx 1. Common w/anthracycline Abx (esp. Doxorubicin), but can occur with any a. Others: 5-FU/capecitabine, dactinomycin, hydroxyurea, methotrexate, paclitaxel vi. Fetus (absolute contraindication!) 2. Compare and contrast cell cycle specific (CCS) and cell cycle non-specific drugs. a. CCS (esp. plant alkaloids and antimetabolites) – act only during a specific portion of the cell cycle, are least effective at treating cancers that have low growth fractions (i.e. most cells are in G0) b. CCNS: (esp. alkylating agents and some natural products) 3. Describe the cell kill hypothesis and its implications for treatment. Develop an appreciation for scheduling and for dosing regimens used to eliminate cancer cells. a. CCS drugs follow 1st order kinetics: kills a constant proportion of tumor cells populations (not constant #) b. Used for acute leukemia, aggressive high-grade lymphomas c. Magnitude follows log function d. Critical points: i. Start early, keep going until cancer can no longer be detected, use approp schedule & sufficient log-kill 4. List the factors that influence the success of chemotherapy and relate those factors to drug administration and choice of antineoplastic agent. a. Cancer: growth fraction (% cells not in G0), doubling time, type, stage, resistance b. Patient: Perf status, BM capacity, liver/kidney function, age, compliance 5. List the generic mechanisms for antineoplastic drug resistance and the factors that contribute to the development of resistance. Be able to give examples of primary, acquired and multidrug resistance. a. Mechanisms: i. Alterations that affect MOA of drugs: (DNA repair, formation of trapping agents, changes in target proteins) ii. Alterations that affect drug concentration inside the tumor cell (action of prodrugs, inactivation, accum) 1 b. Causes of Resistance: i. Poor drug distribution, sanctuary site (esp. brain), tumor cells not in cycle, heterogeneity of tumor cells clonal selection c. Definitions: i. Primary resistance: when some inherent characteristic of the Ca cells prevents the drugs from working ii. Acquired resistance: when Ca cells become resistant during Tx iii. Multidrug resistance: when tumor cells become cross resistant to a wide range of chemically dissimilar agents after exposure to a single (usually nature product) drug. d. MDR: expression of: i. Mdr-1 gene P-gp (can be reversed by Ca2+ channel blockers) ii. MDR proteins (MRP1-9) iii. Lung resistance protein (LRP) 6. List the major mechanisms of action (including any submechanisms) of antineoplastic drugs, and be able to give at least one example of a drug that fits into each category. Be able to do the same type of listing for chemical classes, cell cycle specificity, causes of resistance and major toxicities. NB. This is an objective that you will have to build on throughout this series of lectures. It may be addressed best by looking at the summary tables. a. Flashcards! II. Antimetabolites 1. Chart the specific enzymes and pathways that are blocked by antimetabolite cancer drugs. Be able to identify the specific mechanisms of actions of all drugs that prevent DNA synthesis. 2 1. Folate Biochemistry (MTX, Premetrexed) 2. Pyrimidine Synthesis (5-FU, Capectiabine) a. UMP TMP = rate limiting step in DNA synthesis (cat: thymidylate synthase) b. Resistance to 5-FU: UMP UDP (pyr mono-P kinase) c. Sensitivity to 5-FU: dihydropyrimidine dehydrogenase catalyzed rxn 3. Purine Synthesis (6-MP, 6-TG) a. 1st committed step = formation of 5-P-ribosylamine (enz = PRPP glutamyl amidotransferase) b. 6-MP, 6-TG: inhibit guanylyl kinase pseudo-FB inhibition of PNP/PRPP c. Degraded by conversion of IMP uric acid i. Enz = xanthine oxidase (inhibited by allopurinol) 4. Conversion of ribonucleotides to deoxyribonucleotides (hydroxyurea) a. Enz = ribonucleotide reductase 2. Contrast the mechanisms of action of methotrexate vs. pemetrexed, and identify the mechanisms that make cancer cells more susceptible than normal cells to these drugs (selective toxicity), and understand the principles and advantages of leucovorin rescue. a. Both = competitive inhibitors of DHFR & folate-dep enz of purine and thymidylate synthesis i. MTX depletion of cellular TH4 stores ii. PEM = better antagonist of thymidylate synthase & of purine synth than it is of DHFR b. Net result: inhibition of DNA synth by blocking both purine and deoxythymidylate synthesis, methionine synthesis, AA metabolism c. Both need to have glutamates added to be effective! i. Ca cells are more susceptible to these drugs b/c they are more capable of polyglutamating MTX selective toxicity d. Leucovorin + MTX SE of intense MTX therapy (normal tissues can bypass TH4 synth pathways, which gets around inhibiting DHFR (sel tox) – some Ca cells don’t express a functional reduced folate carrier and cannot take up Leucovorin i. Net result: can use more MTX (get antitumor action with resistance) ii. FATAL if given intrathecally! 3. Compare and contrast the mechanisms underlying the development of resistance to methorexate, 5‑ fluorouracil, 6-mercaptopurine and 6-thioguanine. a. MTX: (use Pemetrexed for cells res to MTX) i. Changes in target enzymes (DHFR) 1. Production of DHFR with a decreased affinity 2. Increased DHFR expression 3. Decreased formation of poly-G/MTX ii. Drug accumulation d/t impaired transport (d/t expr of reduced folate carrier) b. 5-FU i. Changes in target enzymes 1. Increased expression of thymidylate synthase ii. Decreased activation of prodrugs 1. Decreased pyrimidine monophosphate kinase activity c. 6-MP & 6-TG: i. Changes in target enzymes 1. Decreased ability to inhibit PNP and HGPRT ii. Decreased activation of prodrugs 1. Decreased expression of activation enzymes (esp. HGPRT) iii. Increased inactivation 1. Increased rates of degradation of the drugs or their "activated" analogues 3 4. Identify the unique activation mechanisms for 5-fluorouracil, capecitabine and the purine analogues. a. 5-FU i. Needs to be activated (by entering pyrimidine synth pathway) 1. Key entry point = UMPUDP (cat = pyr mono-P kinase) ii. Given IV (degraded by dihydropyimidine deH in the gut) iii. Lots of metabolic degradation (by liver and kidney) b. CAP: i. Oral ii. Converted to 5-FU: 3 steps 1. 1st 2 in liver, last cat by thymidine phosphorylase (overexpressed in tumors) c. Purine Analogues (6-MP, 6-TG) i. Oral, activated by HGPRT ii. 6-MP: 2 pathways in liver 1. 6-MP 5-thiouric acid (inactive) enz = xanthine oxidase a. Adjust dose w/Allopurinol! 2. Methylation / oxidation iii. 6-TG: can be used with Allopurinol 5. Identify the common and unique side effects of methotrexate, 5-fluorouracil and 6-mercaptopurine a. MTX: i. Primary toxic effects are on bone marrow (danger of spontaneous hemorrhage or lifethreatening infection) and GI epithelium ii. Mucositis, myelosuppression and thrombocytopenia - reach their maximum in 5-10 days, and decrease rapidly thereafter iii. Pneumonitis (cough, fever and interstitial infiltrate) iv. Hepatic fibrosis v. Alopecia, dermatitis vi. MTX is abortifacaent b. 5-FU i. 5-FU has a low therapeutic index ii. Primary toxic effects are on bone marrow (danger of spontaneous hemorrhage or lifethreatening infection) and GI epithelium iii. Myelosuppression reaches maximum in 9-14 days iv. Acute cerebellar syndrome (somnolence, ataxia of trunk or extremities, unsteady gait, slurred speech, nystagmus) v. Occurs within weeks/months of initiating treatment in 5% of patients vi. Complete recovery following cessation of treatment vii. Alopecia, dermatitis viii. Hand-foot syndrome (palmar-plantar erythrodysesthesia) 4 c. 6-MP i. Primary toxic effects are on bone marrow ii. Anorexia, nausea and vomiting occur in 25% of adults; less often in children iii. As with any drugs used to treat leukemias, can cause TUMOUR LYSIS SYNDROME 6. Differentiate between the mechanisms of action of the antimetabolite agents that block nucleotide synthesis vs. those that act on DNA synthesizing enzymes. 7. What is tumor lysis syndrome? How can its effects be minimized? Explain the concerns related to co-administration of allopurinol and 6-MP. a. TLS is caused by the sudden, rapid death of millions of cells - a particular problem in successful treatment of patients with leukemia or lymphoma. It results from the development of electrolyte and metabolic disturbances that can produce life-threatening complications (esp. hyperuricemia) if not managed appropriately. b. Prevent hyperuricemia with Allopurinol (=xanthine oxidase inhib) (w/ any drug that causes TLS) c. Allopurinol + 6-MP 6-MP toxicity (b/c 6-MP is metab by xanthine oxidase) i. Need to dose of 6-MP 25-30% normal III. Drugs that disrupt DNA 1. Outline the mechanism of action and the cell targets for crosslinking agents. Understand why these agents are CCNS & why they are particularly beneficial in the Tx of the majority of human cancers. a. Mechanism (alkylating agents) i. Must be/become strong electrophiles ii. Attack on cell nucleophiles iii. DNA damage (crosslinking, miscoding of DNA bases, DNA strand breakage) b. These are CCNS b/c the alkylation rxns that initiate cell death can occur during any phase. i. (Primary toxicity in late G1/S; cell cycle arrest happens in G2) c. Selective toxicity: DNA damage checkpoint (dependent on p53), damage is repaired. Cancer cells (50%) don’t have p53, so these drugs are more effective w/these cancers. 2. Identify the steps in the activation process of cyclophosphamide, and describe how this relates to its specific toxicity and the use of MESNA. What are the implications of this activation process on drug interactions between cyclophosphamide and inducers/inhibitors of CYP2B6? a. Activated by CYP450 b. Final step active drug (phosphoramide mustard) + acrolein (latter = responsible for toxicity: hem cystitis. Need to remove acrolein with MESNA) c. Ind/inhib of cyp2b6 by other drugs have opp effect on cyclophosphamide (induction of enz activity) 3. Identify the toxicities that are common to all crosslinking agents. List the unique properties for each crosslinking agent. (greatest for mechlorethamine, less for oral agents) a. Moderate to severe myelosuppression b. Severe nausea and vomiting c. Strong vesicant properties (not for oral agents) d. Immunosuppression 5 e. Gonadal failure (sterility) f. Carcinogeneisis (leukemia) g. Mutagenesis h. Teratogenesis 4. Compare the cytotoxic and secondary mechanisms of action of the anthracycline antibiotics. Relate these actions to the specific toxicities associated with these drugs. Define the characteristics (both acute and long-term) of the cardiomyopathy associated with dauno- and doxo-rubicin. a. Primary mechanism: intercalation in major groove of DNA causing several cytotoxic actions: i. Inhibition of topoisomerase II ii. Single- and double-strand breaks (mutagenic) or sister chromatid exchange (carcinogenic) iii. DACTINOMYCIN binds to DNA via an alkylation reaction blocks RNA polymerase more than DNA polymerase b. Secondary mechanisms: i. Interact with cell membranes to alter fluidity and ion transport ii. In the presence of NADPH, react with cytochrome P450 reductase to form superoxide anion radicals; also causes unique cardiotoxicity iii. CCNS, but maximal toxicity in S phase (at low concentrations will pass through S and die in G2) c. ANTHRACYCLINE ANTIBIOTICS cause an UNUSUAL CARDIOMYOPATHY that is often IRREVERSIBLE and related to the TOTAL DOSE of the drug 1. May be due to production of free radicals within the myocardium - theoretically, can be partially reduced by using exogenous antioxidants to boost normal cell defenses ii. Cardiomyopathy: 1. Acute: increased heart rate, conduction abnormalities, arrhythmias 2. Delayed: congestive heart failure that is unresponsive to digitalis (may occur years after treatment) iii. Extravasation necrosis (vesicant) iv. Myelosuppression is major dose-limiting complication (individual course of treatment) v. Nausea and vomiting vi. Alopecia vii. Mutagenic, carcinogenic viii. "Radiation recall reaction" - erythema and desquamation of the skin at sites of prior radiation therapy ix. Hand-foot syndrome (palmar-plantar erythrodysesthesia) x. Red urine 5. Identify the resistance mechanisms for each of these agents, and be able to identify situations where multidrug resistance is likely to develop. (flashcards) a. MDR: Increased expression of: i. MDR-1 gene à increased levels of P-glycoprotein 1. Experimentally, calcium channel blockers (e.g. verapamil) can reverse this resistance ii. Multidrug resistance proteins (MRP1-9) iii. Lung resistance protein (LRP) 1. This is a common resistance mechanism for natural products (e.g., plant alkaloids, anthracylcine antibiotics) 6. Categorize the agents that cause strand breaks in terms of their specific mechanisms of action, and their chemical classes. Identify the unique properties of bleomycin that make it a useful component of many drug regimens. a. Mechanisms: all are CCS; all require functional apoptotic machinery (esp. p53) to complete the cell kill b. Chem classes: i. Antibiotic: BLEOMYCIN ii. Plant alkaloids: 1. Epipodophyllotoxin: ETOPOSIDE 2. Camptothecin: IRINOTECAN 6 iii. Miscellaneous: PROCARBAZINE c. BLEOMYCIN BLASTS DNA i. Unique mechanism and toxicities, included in many combination regimens ii. BLEOMYCIN binds to DNA (not RNA) through its amino-terminal peptide, and generates free radicals that cut the DNA iii. Causes accumulation of cells in G2 that have chromosomal aberrations (chromatid breaks, gaps, fragments and translocations) IV. Antimitotics & Immune System Modifiers 1. Identify the differences in mechanism of action and development of resistance among the various types of antimitotic drugs. Distinguish between the toxicities of vincristine and vinblastine. a. Taxanes (Paclitaxel) i. MOA: bind to tubulin and ENHANCE AND STABILIZE spindle assembly ii. RES: decreased accumulation via increased P-glycoprotein expression àMDR b. Abx: Epilone: Ixabepilone i. MOA: antibiotic that binds to tubulin and ENHANCES AND STABILIZES spindle assembly (similar to PACLITAXEL) ii. Is not limited by development of multidrug resistance (unlike vinca alkaloids and PACLITAXEL) iii. Used in combination with CAPECITABINE for the treatment of metastatic breast cancer following treatment failure with an anthracycline antibiotic and PACLITAXEL (i.e., it is a 3rd line treatment) iv. Metabolized in the liver v. Causes bone marrow suppression (esp. neutropenia), peripheral neuropathy and cardiac arrhythmias vi. Can also produce hypersensitivity reactions c. As a class, vinca alkaloids are recognized as being agents that cause bone marrow suppression and neurotoxicity, although VINBLASTINE and VINCRISTINE cause these toxicities to differing degree i. Mneumonic: 1. VINCRISTINE = CNS toxicity (more lipid soluble, fatal if given intrathecally) 2. VINBLASTINE = bone marrow suppression ii. Bone marrow suppression (greater for VINBLASTINE) iii. Nausea and vomiting (greater for VINBLASTINE) iv. Vesicant (common toxicity of many cytotoxic agents) v. Neurotoxicity (greater for VINCRISTINE) 1. Prominent because of the requirement for microtubules in axon transport 2. Common symptoms: a. Motor: loss of reflexes b. Autonomic: constipation, paralytic ileus, orthostatic hypotension c. Sensory: paresthesias ("pins and needles") 3. Depression of deep tendon reflexes occurs within 2-3 weeks in 100% of patients, because this is used as an indication of sufficient dose 4. This can be followed by severe paresthesias and mild to moderate sensory loss (an indication to decrease the dose) vi. Alopecia 2. Describe differences in the use of glucocorticoids and selected antibiotics for cancer chemotherapy vs. immunosuppression. Trigger for cell division Cancer cells Normal immune system Unstimulated Specific antigen 7 Cell division Drug administration Random Synchronized Chemotherapy Immunosuppression High dose, "pulse" Low dose, continuous 3. Name the cytokines that have been approved for use in cancer treatment. Identify the aspects of their pharmacokinetics and toxicities that are common among this class of drugs, as well as their unique side effects. a. IL-2, INF-a, TNF-a b. Common PK/Tox i. Short t1/2, aren’t cytotoxic by themselves (recruit immune cells to actually kill the cell) c. Unique side effects: i. IL-2: 1. Activation and expansion of lytic lymphocytes causes inflammation, vascular leak and secondary release of other cytokines (such as TNF, interferon α) 2. Can produce mild/moderate symptoms such as fever/chills, diarrhea and weight gain or hand-foot syndrome (palmar-plantar erythrodysesthesia) 3. Serious toxicities such as thrombocytopenia, shock, respiratory distress, coma and fatal hypotension ii. INF-a: 1. Flu-like symptoms: fever, arthralgias, headache, fatigue 2. Hypotension 3. Myelosuppression 4. Depression iii. TNF-a: 1. Severe dose-limiting toxicity is malaise and flu-like symptoms a. Can cause hemorrhagic necrosis 4. Be able to match the monoclonal antibodies used in cancer treatment to their targets and to their unique, serious side effects. TARGET DRUG USE RITUXIMAB CD20 IBRITUMOMAB (90Y) B-cell non-Hodgkin's lymphoma (NHL) TOSITUMOMAB (131I) CD33 GEMTUZUMAB acute myeloid leukemia (AML) CD52 ALEMTUZUMAB B-cell chronic lymphocytic leukemia (B-CLL) EGFR CETUXIMAB metastatic colon cancer 17-1A EDECOLOMAB colon cancer HER2 TRASTUZUMAB metastatic breast cancer VEGF BEVACIZUMAB discussed under antiangiogenesis 8 V: Drugs that interfere w/protein function (CML module) 1. Be able to categorize drugs that inhibit protein function with respect to the specificity of the processes that they target a. Signal transduction inhibitors: DASATINIB, ERLOTINIB, GEFITINIB, IMATINIB, LAPATANIB, NALOTINIB, SORAFENIB, SUNITINIB b. L-ASPARAGINASE c. Proteosome inhibitor: BORTEZOMIB d. HDAC inhibitor: VORINOSTAT i. At one end are drugs that target a unique aspect of a specific cancer type (such as LASPARAGINASE and IMATINIB); ii. Less specific are those that exploit overexpression of a particular protein (such as ERLOTINIB and GEFITINIB); iii. And at the other end are drugs that are really targeting rapidly dividing cells and/or angiogenesis (like BORTEZOMIB, VORINOSTAT, SORAFENIB and SUNITINIB). 2. Describe the mechanisms of action and side effects of the currently approved signal transduction inhibitors, and explain the success of imatinib vs. gefitinib. a. MOA: b. DASATANIB, IMATINIB (Gleevec), NILOTINIB i. Competitive antagonists of the ATP-binding site of: 1. bcr-abl, the non-receptor tyrosine kinase whose activity is deregulated by the translocation of its gene from chromosome 9 to chromosome 22 in most patients with CML 2. Also target c-kit, the tyrosine kinase altered in gastrointestinal stromal tumours (GIST), and are weak antagonists of the platelet-derived growth factor (PDGF) receptor 3. DASTAINIB also targets Src, a tyrosine kinase whose expression is upregulated in several types of cancer a. May be anti-metastatic in epithelial-derived tumours c. ERLOTINIB (Tarceva/Genetech), GEFITINIB (Iressa/AstraZeneca) i. Competitive antagonists of the ATP-binding site of epithelial growth factor receptor (EGFR) tyrosine kinase, which is over-expressed in a large number of epithelial-derived cancers d. LAPATINIB i. Competitive antagonist of the ATP-binding site of EGFR and HER2 (dual inhibitor) e. SORAFENIB, SUNITINIB i. Antagonist of multiple kinases, including VEGF-R, PDGF-R as well as: 1. SORAFENIB: Ras 2. SUNITINIB: c-KIT ii. Net result is a decrease in angiogenesis f. Side effects: g. Generally, relatively minor side effects (compared to conventional therapies): nausea, vomiting, fatigue, myalgia, diarrhea, skin rashes and acne, drug interactions h. Can cause congestive heart failure and decreased left ventricular ejection fraction (causing shortness of breath, palpitations, fatigue) and/or myocardial infarction i. Incidence and severity vary widely within this group (more common and more severe with IMATINIB, less so with LAPATANIB, for example) 9 i. j. k. l. m. Teratogenic IMATINIB: edema, bone marrow suppression ERLOTINIB and GEFITINIB: interstitial pneumonia (which can be fatal) SORAFENIB: increased risk of hemorrhage, hypertension SUNITINIB: skin discoloration, hand-foot syndrome (palmar-plantar erythrodysesthesia) Imatinib vs. Gefitinib: Understanding of the genetic defects Homogeneity of disease process among candidate patients ("likely responders") Uniqueness of drug target (molecular markers) Large scale success IMATINIB (CML) GEFITINIB (NSCLC) Excellent Poor Yes, among patients in chronic phase No Only in cancer cells In many normal and cancer cells Yes Not really (fails more often than it works) 3. Contrast conventional therapy for the treatment of CML with the use of STIs with respect to cure rates, remission and side effects. a. IMATINIB i. Can induce a complete hematological and cytological response in 85-95% of patients in the chronic phase of CML ii. Can delay death in 25% of patients in blast crisis (75% of these patients initially respond) iii. Also effective in gastrointestinal stromal tumors expressing c-kit b. ERLOTINIB, GEFITINIB i. Use: metastatic non-small cell lung cancer (NSCLC) after failure of standard chemo ii. Different populations experience varying efficacies: 1. 25% of NSCLC cases in Japan respond, but 10% of cases in US 2. Non-smokers and broncho-alveolar subtype do better iii. Having the "right" mutation (and we don't know what that is) means the difference between a "cure" and no response c. LAPATANIB: with CAPECITABINE for patients with metastatic breast cancer where treatment with an anthracycline, taxane and TRASTUZUMAB have failed d. SORAFENIB, SUNITINIB : advanced renal cell carcinoma as well as: i. SORAFENIB: hepatocellular carcinoma ii. SUNITINIB: imatinib-resistant GIST iii. These drugs are highlighted in the controversy over the high cost of new cancer treatments 4. Understand the mechanisms of action of L-asparagine, bortezomib and vorinostat. Be aware of the reasoning behind the sequence of administration of L-asparagine and methotrexate. Contrast the side effects of the bortezomib and vorinostat with conventional cytotoxic drugs. a. MOA: b. L-Asparaginase: i. In normal cells, the asparagine used for protein synthesis is generated from aspartate by asparagine synthase; asparagine outside the cell is converted to aspartate by LASPARAGINASE before being pumped into the cell and converted back to asparagine ii. Administration of L-ASPARAGINASE causes selective toxicity because some tumour cells lack asparagine synthase (i.e., they require an exogenous sources of L-asparagine for protein 10 synthesis), therefore decreasing the asparagine concentration by giving L-ASPARAGINASE deprives tumour cells of asparagine iii. Used to treat childhood acute lymphocytic leukemia iv. Main side effects are hypersensitivity reactions (fever, chills, nausea/vomiting, skin rash and urticaria) because L-ASPARAGINASE is isolated from bacteria v. Usually used with other agents; sequence of drug administration is critical, for example: 1. If METHOTREXATE is given first, you have synergistic cytotoxicity 2. If L-ASPARAGINASE is given first, the METHOTREXATE cytotoxicity is reduced as METHOTREXATE toxicity is dependent upon synthesis of the enzymes necessary for DNA synthesis c. Bortezomib i. Reversible inhibitor of the 26S proteosome (a large protein complex that degrades ubiquitinated proteins, esp. misfolded proteins) ii. The ubiquitin-26S proteasome pathway regulates the intracellular concentration of proteins, thereby maintaining cellular homeostasis - inhibition of the 26S proteasome affects multiple signalling cascades, leading to cell death iii. The nature of the specific signalling cascades that are affected may confer specificity of BOREZOMIB for cancer vs. normal cells, and determine its effectiveness in one type of cancer vs. another d. Vorinostat: i. Histone deacetylases (HDACs) work in conjunction with histone acetyltransferases to regulate gene expression 1. acetylation is associated with euchromatin ("open for transcription") 2. deacetylation is associated with heterochromatin ("closed") ii. Some cancer cells overexpress or aberrently recruit HDACs, leading to hypoacetylation of histones, condensed chromatin structure and decreased transcription 1. Causes silencing of tumor suppressor genes (esp. p53) iii. HDAC inhibitors increase transcription, and lead to cell cycle arrest and apoptosis iv. valproic acid (a 1st generation HDAC inhibitor that is approved for use as a mood stabilizer and as an antiepileptic) is under investigation for use in cancer 1. HDAC inhibitors are under active investigation for use in Huntington's disease & ALS v. VORINOSTAT is approved for use in cutaneous T-cell lymphoma, and is under investigation in glioblastoma multiforme and HIV vi. VORINOSTAT undergoes hepatic metabolism (but not by CYP450), and it is not a substrate for P-glycoprotein e. Side effects of Bortezomab vs. Vorinostat: i. BORT: thrombocytopenia, neutropenia and/or anemia; peripheral neuropathy ii. VOR: 1. HEMATOLOGIC: pulmonary embolism, deep vein thrombosis, thrombocytopenia and anemia 2. DRUG/DRUG INTERACTIONS: a. Severe thrombocytopenia and GI bleeding result from coadministration with valproic acid b. PT and INR are prolonged if given with WARFARIN 3. Nausea, vomiting, diarrhea 4. Hyperglycemia (esp. in diabetics) 5. Fatigue, chills 6. Taste disorders (dysgeusia, dry mouth) 7. Mutagenic (carcinogenic?) 11 VI: Angiogenesis inhibitors, differentiating agents, & Combination Chemotherapy 1. Explain the role of naturally occurring angiogenesis inhibitors in the growth of secondary tumors following surgery. Describe the mechanisms of action and side effects attributed to bevacizumab and thalidomide. a. Role of Naturally Occurring Angiogenesis Inhibitors: b. All tissues (including tumors) secrete substances that promote or inhibit angiogenesis (the formation of new blood vessels) - more than 35 angiogenesis stimulators & 18 suppressors described c. Once a group of cancer cells reaches a certain size (~1-2 mm in diameter), it must develop a blood supply in order to grow, because diffusion is no longer adequate to supply the cells with oxygen and nutrients and to take away wastes d. Some tumors secrete substances that inhibit angiogenesis at other tumor sites which leads to the clinical phenomenon whereby: i. Pt has a primary tumor, and there is no evidence that the primary tumour has metastasized ii. A surgeon removes the primary tumour iii. Some weeks later, metastases of the tumour appear throughout the patient's body. e. The speed of the appearance of the secondary tumours indicates that they were present all along, but were too small to be detected (this is one of the justifications for chemotherapy as an adjunct to surgery for the treatment of solid cancers) f. MOA and Side Effects of Bevacizumab and Thalidomide: i. Bevacizumab: 1. humanized monoclonal antibody directed against VEGF 2. Approved (in combo w/ 5-FU) for first-line treatment of patients with metastatic colorectal cancer a. Being investigated for use in many other cancers b. Also approved for use in macular degeneration and diabetic neuropathy i. RANIBIZUMAB (which is promoted by the drug company as the preferred treatment) is a derivative of BEVACIZUMAB 3. In addition to the side effects common to antibodies, BEVACIZUMAB can cause gastrointestinal perforation, wound dehiscence and hemoptysis, which can be fatal 4. There is concern that BEVACIZUMAB treatment could worsen coronary or peripheral artery disease by preventing the sprouting of new vessels ii. Thalidomide: 1. = Developmental toxin 2. Approved for use in Tx of Hansen’s disease. Off lab used: AIDS Tx, multiple myeloma 3. SE: Severe birth defects (esp. phocomelia) 2. Define the mechanisms of action and characteristic toxicities of tretinoin, arsenic trioxide and bexarotene. a. Tretinoin: i. In APL, activates the differentiation program and promotes degradation of the PML-RAR fusion gene (also used to treat acne (gel form)) ii. Toxicities: 1. dry skin, reversible hepatic enzyme abnormalities, bone tenderness, hyperlipidemia; 2. RETINOIC ACID SYNDROME: fever, dyspnea, weight gain, pulmonary infiltrates a. with or without pleural or pericardial effusions b. with or without leucocytosis 3. birth defects (teratogenic) b. Arsenic Trioxide (ATO) i. Heavy metal toxin that is thought to induce differentiation and promotion of apoptosis (although it has many other cytotoxic effects) ii. Approved for relapsed APL (complete responses in 85% of patients) iii. Generally well tolerated, but toxicities include: 12 1. Arrhythmias (prolongation of QT interval) 2. Leukocyte maturation syndrome similar to retinoic acid syndrome c. Bexarotene: i. Rexinoid that selectively binds to retinoid X receptors (nuclear receptors that are involved in the regulation of cell growth and differentiation) ii. Approved for use in patients with cutaneous T-cell lymphoma that is refractory to skindirected treatment iii. Metabolized by CYP3A4 (potential for many drug interactions) iv. Side effects include: GI symptoms, lipid abnormalities and pancreatitis (must monitor blood lipid levels) v. TERATOGENIC 3. List the advantages of combination chemotherapy and understand the strategies used to design chemotherapy drug regimens. Apply these concepts to the commonly used combination therapies for the treatment of Hodgkin’s disease, non-Hodgkin’s lymphoma, testicular carcinoma and breast cancer. a. Combination chemotherapy / Strategies of designing drug regimens: i. Principles of drug selection: 1. Active when used alone 2. Different mechanisms of action (including different mechanisms for the development of resistance) and/or different chemical classes 3. CCNS vs. CCS or active in different stages of cell cycle 4. Different toxicities ii. Enables use of more specific strategies (recruitment and synchrony) iii. Can result in: 1. Synergistic effects (effect greater than the sum of the actions of the individual drugs); lower doses decreased toxicity a. e.g., CYTARABINE + 6-THIOGUANINE 2. Decreased development of resistance REGIMEN MECHANISM OF RESISTANCE ACTION MECHANISMS UNIQUE (PRIMARY) TOXICITY ABVD for Hodgkin's disease Adriamycin CCNS = Doxorubicin Intercalating agent Bleomycin Vinblastine Dacarbazine CCS (G2) Strand breaks CCS (M) Antimitotic P-glycoprotein Changes in target Increased inactivation Increased DNA repair; Increased inactivation P-glycoprotein CCNS Nucleophile production Alkylating agent Increased DNA repair 13 Cardiotoxicity Myelosuppression Skin and lungs (not myelosuppression) Neurotoxicity Myelosuppression Myelosuppression MOPP for Hodgkin's disease: Mechlorethamine, Oncovin = vincristine, Prednisone, Procarbazine COP (+/-D = CHOP) for non-Hodgkin's lymphoma Cyclophosphamide, Oncovin = vincristine, Prednisone, Doxorubicin PVB for testicular cancer Platin (carbo- or cis-), Vinblastine, Bleomycin FAC for breast cancer 5-Fluorouracil, Adriamycin = doxorubicin, Cyclophosphamide CMF for breast cancer Cyclophosphamide, Methotrexate, 5-Fluorouracil 4. Define the terms pulse therapy, recruitment, synchrony, and rescue. Be able to give examples of each type of treatment. a. Pulse Therapy: intermittent treatment with very high doses of a drug i. Allow hematologic and immunologic recovery between treatment cycles ii. Example: METHOTREXATE for the treatment of choriocarcinoma b. Recruitment: use a CCNS drug to achieve a significant log kill i. This will cause cancer cells in G0 to be recruited back into the cell cycle ii. Administer a CCS drug to kill dividing cells 1. Examples: CMF in breast cancer; DAUNORUBICIN + CYTARABINE in AML c. Synchrony: using CCS drugs to synchronize cells into simultaneous cell division, so that they are more sensitive to other drugs or radiation i. Timing the delivery of drugs so that the action of one drug doesn't interfere with the actions of another ii. Examples: 1. HYDROXYUREA followed by radiation 2. VINCA ALKALOIDS (M phase) followed by another CCS drug like ETOPOSIDE (S phase) 3. METHOTREXATE followed by L-ASPARAGINASE for the treatment of acute lymphocytic leukemia d. Rescue: following administration of toxic doses of a chemotherapeutic agent, normal cells can be rescued by giving "antidotes" that only they can use i. Example: LEUCOVORIN following high dose METHOTREXATE treatment Folate, Vit B12 & Inhibitors: 1. Be able to describe the specific functions of FOLIC ACID and VITAMIN B12, and relate these functions to the inhibition mediated by METHOTREXATE and TRIMETHOPRIM. a. Folate and vitamin B12 are required for DNA synthesis and for maintenance of neurons and RBCs b. Folate is the critical precursor in the neosynthesis of tetrahydrofolate (TH4) i. TH4 is a 1 carbon donor in several reactions including: 1. Thymidylate and purine synthesis 2. Methionine synthesis 3. Amino acid metabolism c. Vitamin B12 is an intermediate in: i. A reaction that converts methylTH4 (the primary stored form of TH4) to TH4 1. In the process, homocysteine is converted to methionine (homocysteine levels are decreased as a result) 14 2. The conversion of methylmalonyl CoA to succinyl CoA d. MTX: i. Competitive inhibitor of dihydrofolate reductase (DHFR) ii. Therapeutic uses: 1. Cancer (1st solid tumour cure – choriocarcinoma) 2. Immunosuppressant: rheumatoid arthritis, psoriasis, inflammatory bowel disease/Crohn's disease 3. Antibiotic: Pneumocystis jirovecii (an AIDS-associated disease) – bug doesn’t have the reduced folate carrier, which means LEUCOVORIN rescue is effective here also TRIMETREXATE is actually the best antifolate for treatment of Pneumocystis jiroveci 4. Abortifacient: in 1st trimester – typically combined with MISOPROSTROL (PGE1) e. Trimethoprim i. Selective, competitive inhibitor of BACTERIAL dihydrofolate reductase (DHFR) ii. Typically combined with SULFAMETHOXAZOLE (which blocks dihydropteroate synthetase). These drugs act synergistically, blocking successive steps in the folate synthesis pathway in bacteria. 2. Explain the mechanism by which the reduced folate carrier is involved in the differential sensitivity of cancer cells and bacteria to folic acid inhibitors. a. Absence of the reduced folate carrier confers resistance to low doses of folate inhibitors (such as METHOTREXATE), but also allows the design of successful high-dose treatment. Cancer cells or bacteria that do not have this transporter cannot accumulate reduced folates after inhibitor treatment, while normal cells can protect themselves by accumulating other folates (such as LEUCOVORIN). This is the fundamental principle underlying rescue therapy. 3. Know the consequences of FOLATE and VITAMIN B12 deficiency, and strategies for replacement. a. Deficiency of either one prevents DNA synthesis, has bad effects on rapidly growing cells b. Most prominent clinical signs = megaloblastic anemia c. FOLATE i. Deficiency can be caused by: 1. Insufficient dietary intake, high demand (pregnancy), Alcoholism, intestinal disease (sprue), inhibitors ii. Causes megaloblastic anemia iii. Also causes neural tube defects in children born to mothers with low folic acid levels (no neurologic damage in adults) d. VITAMIN B12 i. Most commonly due to a deficiency in intrinsic factor (à can't treat with oral doses) 1. Very rarely caused by a nutritional disorder ii. Vitamin B12 deficiency will cause a folate deficiency by preventing the activation of methyltetrahydrofolate iii. Result is megaloblastic anemia (called pernicious anemia if caused by a impaired B12 absorption) and neurological damage (paresthesias and weakness that progress to spasticity, ataxia and other CNS disorders) 1. Up to 10% of dementia in the elderly is believed to be caused by B12 deficiency 2. Correction of the deficiency can stop progression of the neurological effects but cannot entirely reverse them 15