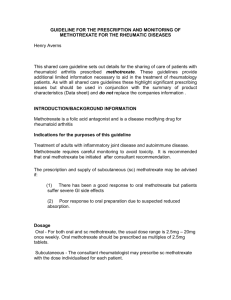
METHOTREXATE TREATMENT FOR PATIENTS WITH IBD
advertisement

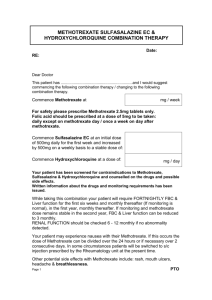
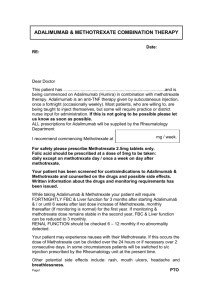
METHOTREXATE TREATMENT FOR PATIENTS WITH IBD PATIENT INFORMATION LEAFLET This information leaflet is designed to answer common questions patients ask about their medicine. Further information can be found in the information leaflet supplied by the manufacturer or from your pharmacist or doctor. Why have I been started on this medicine ? • Methotrexate is a medicine used to induce and maintain remission of Crohn’s disease and Ulcerative colitis in patients who have steroid dependent or refractory disease, or who have been intolerant of either azathioprine or 6-Mercaptopurine. How is it taken ? • In tablet form, weekly or by Intra Muscular injection. Your Gastroenterology team will decide on the appropriate dose for you as well as organizing regular blood tests. To reduce the risk of side effects from methotrexate, you will also be asked to take a vitamin called Folic Acid once a week (that will also be prescribed for you), but you should NOT take this on the same day as the methotrexate treatment. How does it work ? Methotrexatesuppresses inflammation and dampens down the body’s immune system. How long does it take to work ? The benefits of methotrexate treatment often take quite a number of weeks to occur. How long will I be taking it ? Patients who respond to methotrexate usually remain on it for many months and perhaps several years as long as the blood test monitoring remains satisfactory. Do not stop taking your medicine unless your doctor tells you to, however well you feel. What are the common side effects ? Fortunately many patients do not suffer any side effects with this treatment. Some of the common side effects can be reduced by simple measures : • Nausea / vomiting – this is perhaps the commonest side effect likely to occur. These symptoms can often be reduced by taking the drug at a different time of the day – eg on retiring to bed; by ensuring that you are taking the vitamin supplement called Folic acid; for some patients, your Specialist will give you a prescription for an anti-sickness medication to take about an hour before your weekly dose of methotrexate. Other common side effects include : mouth and nasal ulcers; diarrhoea; abdominal pain and bloating; fatigue; symptoms of a cold / flu like illness; joint pain; insomnia; facial flushing; eye irritation; dizziness; mild hair loss; loss of libido / impotence; decreased fertility (reversible on completion of treatment). Other rare side effects include : headache; acne; skin irritation and itching; increased sensitivity to light; tingling / numbness; dry cough and / or shortness of breath. Should you develop any of these troublesome symptoms you should report them to your specialist Gastroenterology team. Special monitoring You will need to undertake a pre treatment screening. The results of which will ensure suitability. Blood tests will be taken at regular intervals throughout administration of the drug. • Do not receive any live vaccines (rubella, polio). • Avoid contact with people who have infections. • Avoid pregnancy. • Contraception is strongly recommended. • If breastfeeding, this should be stopped as methotrexate passes into breast milk. • In certain patients, liver biopsy may be required if treatment is ongoing. Methotrexate and pregnancy Do not become pregnant whilst taking methotrexate treatment. Because methotrexate may damage sperm, adequate birth control is essential for both men and women. Contraception (for both sexes) should be continued for at least 3 months after stopping methotrexate treatment. Keep all medicines out of the reach of children. Never give any medication prescribed for you to anyone else. It may harm them even if their symptoms are the same as yours. For further information you can contact your IBD Nurse Specialist or Gastroenterology specialist.