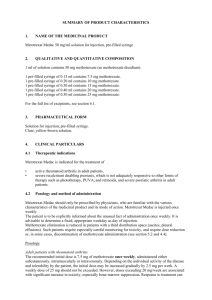
METHOTREXATE - British Society of Gastroenterology
advertisement

METHOTREXATE Introduction : Methotrexate is an immunomodulator used to induce and maintain remission of Crohn’s disease and Ulcerative colitis in patients who have steroid dependent or refractory disease, or who have been intolerant of either azathioprine or 6-Mercaptopurine. Methotrexate inhibits the enzyme dihydrofolate reductase, essential for the synthesis of purines and pyrimidines. Although unlicensed to treat inflammatory bowel disease, methotrexate is widely used in Crohn’s disease (BNF section 1.5) and less commonly in ulcerative colitis. Dose and mode of administration : Much of the evidence for the beneficial effects for methotrexate has been with the intramuscular route of administration. The evidence for the efficacy and bioavailability of oral methotrexate is limited in Crohn’s disease, although there is very good evidence for its efficacy in the treatment of Rheumatoid Arthritis for over 50 years. Many Gastroenterologists are now recommending oral therapy as it is more convenient for the patient and easier to supervise. Intramuscular route : 25mg once per week for up to 16 weeks, then reduced to 15mg once a week. Oral route : Intially 15mg once per week as a single dose, increasing to 20mg once per week after 2 weeks and up to a maximum of 25mg once a week after a further 2 weeks as tolerated and according to response. A lower starting dose may be required for the elderly or frail or those with renal impairment. Clinical response is usually evident in 4-6 weeks. Folic acid treatment : Folic acid reduces the toxicity of methotrexate treatment and improves continuation of therapy and compliance. Folic acid should be taken ONCE weekly, but SHOULD NOT be taken on the same day as the methotrexate. Recommended monitoring and precautions / interactions Monitoring Schedule : Pre-treatment assessment British Society of Gastroenterology recommendation Avoid use in patients with known liver disease (including fatty liver), alcohol excess, obesity, diabetes or women trying to conceive. Monitoring FBC, U&E, LFT’s Pre-treatment Pulmonary Function Tests and CXR may be considered for some patients FBC, U&E, LFT’S every 2 weeks after the last dose change; thereafter monthly until stabilised. Monitoring frequency every 2-3 months if patients results remain stable Action to be taken : WBC < 3.5 x 109/l Neutrophils < 2.0 x 109/l Platelets < 150 x 109/l Withold treatment and recheck in 1 week Discuss with Specialist team Withold treatment and recheck in 1 week Discuss with Specialist team Withold treatment and recheck in 1 week Discuss with Specialist team MCV > 105fl Check serum B12, folate & TFT and Discuss with Specialist team AST, ALT > 2 fold rise (from the upper limit of the reference range) Consider for liver biopsy when persistent elevation occurs. Discontinue treatment in patients with abnormal LFT’s who decline liver biopsy Monitor closely and consider need for liver biopsy Nausea occurs commonly & may be reduced by changing timing of dose (before bedtime), ensure adequate intake of folic acid, & consider antiemetic at time of weekly dose Albumin – Unexplained fall in the absence of active disease Nausea Rashes or oral ulceration, vomiting & diarrhoea Renal function – significant deterioration compared to baseline or upper limit of normal of reference range Severe sore throat, abnormal bruising New or increasing dyspnoea or dry cough Withold treatment and recheck in 1 week Discuss with Specialist team Withold treatment and recheck results Discuss with Specialist team Immediate FBC and withhold until the result of FBC is available Withold treatment; CXR & pulmonary function tests; Discuss with Specialist team The incidence of hepatotoxicity in patients with inflammatory bowel disease is very low and particularly so, if the drug is only given to carefully selected patients – avoiding its use in : In patients suspected of alcohol abuse; The Obese Patients with previously demonstrated fatty liver, pre-treatment abnormalities of liver function and those with pre-existing liver disease Liver biopsy should be considered when there is a persistent elevation of the transaminases above baseline or a decrease in the albumin level below the reference range when the inflammatory disease is inactive. Methotrexate is contraindicated in patients with significant renal impairment because the primary mode of excretion of the drug is via the kidneys. Renal toxicity occurs rarely with methotrexate treatment, but cases of nephrotic syndrome and renal failure have been described. Pneumonitis has very rarely been reported in patients with IBD taking methotrexate treatment. If respiratory symptoms develop whilst a patient is receiving methotrexate treatment, a CXR and pulmonary function tests should be arranged urgently and the drug discontinued. Bone marrow suppression may occur as a result of methotrexate treatment. The risk is greatest in the elderly and those with significant renal impairment. When a significant fall in the indices has occurred the following should be arranged immediately : Stop Methotrexate therapy Give Folinic Acid Rescue – The initial dose should be at least 20mg given intravenously. Subsequent doses of 15mg given orally at 6 hourly intervals until the haematological abnormalities have improved (usually not more than 2 – 8 doses. Consider immediate discussion with Supervising Specialist team / Medical On Call team or the local Haematologist. Pregnancy & Breast feeding : Methotrexate is both teratogenic and is an abortofacient. Methotrexate may also be toxic to sperm. Adequate birth control is therefore essential for both men and women. Contraception (for both sexes) should be continued for at least 3 months after stopping methotrexate therapy. Methotrexate may be excreted in breast milk so breast feeding is contraindicated. Should an inadvertent pregnancy occur, referral should me made to an Obstetrician. Cautions : Patients with clinically significant renal impairment from any cause Localised or systemic infection including hepatitis B & C and past history of TB Unexplained anaemia or cytopenia associated with bone marrow failure Immunisation with live vaccines should be avoided (pneumoccocal and Influenza vaccinations can be given) Drug interactions : o Phenytoin, Co-trimoxazole, Trimethoprim – the antifolate effect of methotrexate is increased o Probenacid, Penicillin, Azapropazone, NSAID’s – Methotrexate excretion is reduced (but a clinically significant interaction between methotrexate and NSAID’s is rare o Tolbutamide – serum concentrations of methotrexate may be increased Duration of treatment As for azathioprine, the duration for continuing treatment with MTX cannot be recommended from current literature alone. If well-tolerated, the drug may be continued for several years, under appropriate supervision. Hepatic fibrosis now seems relatively uncommom in these IBD patients, and liver biopsy is no longer routinely recommended after 1.5g intake. Serum markers of fibrosis are available in spcialist centres, if needed. Again, informed discussion with the patient as to the uncertainties of long-term toxicity are necessary, if therapy continues beyond 3-5 years without attempted withdrawal of the drug. REFERENCES 1. Feagan.BG, Rochon.J. et al .Methotrexate for the treatment of Crohn’s disease. The North American Crohn’s study group Investigations.N.Engl.J.Med.1995; 332:292-297. 2.Feagan.BG, Fedorak.R et al. A comparison of methotrexate with placebo for the maintenance of remission in crohn’s disease.N.Engl.J.Med. 2000; 342: 1627-1632. 3. Alfadhli AA, McDonald JW, Feagan BG. Methotrexate for induction of remission in refractory Crohn’s disease. Cochrane Database Syst. Rev. 2005; (1) : CD003459. 4. Hawthorne AB. Methotrexate : a useful alternative in Crohn’s disease ? Gut 2001; 49 : 9-10. 5. Rampton DS. Methotrexate in Crohn’s disease. Gut 2001; 48 : 790-1. 6.Fraser AG, Morton D, McGovern D, Travis S, Jewell DP. The efficacy of methotrexate for maintaining remission in inflammatory bowel disease. Aliiment. Pharmacol. Ther. 2002; 16 : 693-7. 7. Aberra FN, Lichtenstein GR. Review article : monitoring of immunomodulators in inflammatory bowel disease. Aliment. Pharmacol. Ther. 2005; 21 : 307-19. 8. Siegel CA, Sands BE. Review article : practical management of inflammatory bowel disease patients taking immunomodulators. Aliment. Pharmacol. Ther. 2005; 22 : 1-16. 9. Sun JH, Das KM. Low-dose oral methotrexate for maintaining Crohn’s disease remission : where we stand. J. Clin. Gastroenterol. 2005; 39 : 751-6. 10. Kurnik D, Loebstein R, Fishbein E, Almog S, Halkin H, Bar-Meir S, Chowers Y. Bioavailability of oral vs. subcutaneous low dose methotrexate in patients with Crohn’s disease. Aliment. Pharmacol. Ther. 2003; 18 : 57-63.