First Line Anti
advertisement
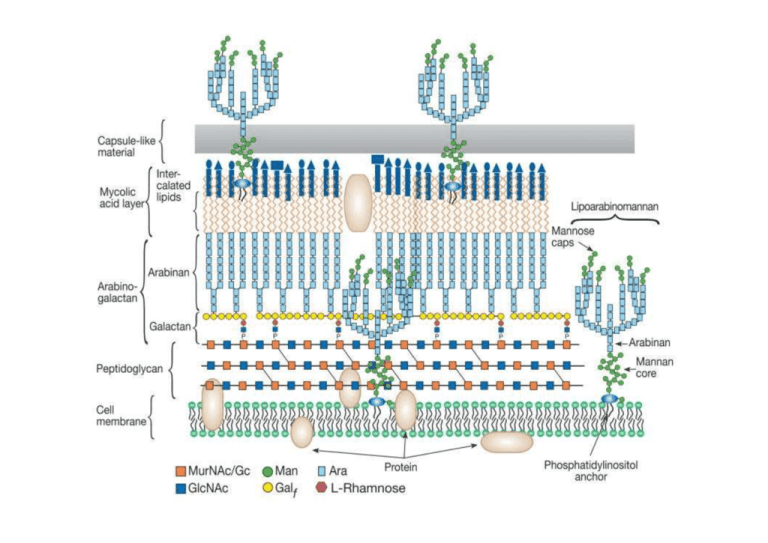
Drugs/Infos Isoniazid (INH) Adsorption 1. Well absorbed orally Distribution 1. Readily distributed in all body fluid 2. Easily reaches Tx level in CSF Metabolism 1. Undergoes 2nd phase of metabolism (Conjugation phase ) 2. Being acetylated by Acetyltransferase in liver. 3. Acetyltransferase expression is highly genetic polymorphism* Excretion 1. Metabolites and unchanged form excreted via urine Tuberculocidal Mechanism of Action Clinical Uses INH is a mycolic acid synthesis inhibitor 1. Activated by Mycobacterial Catalase Peroxidase 2. The activated INH binds covalently with a. Acyl carrier protein b. Beta-ketoacyl carrier protein synthetase 1. One of the two most potent anti-TB drugs Anti-TB Regimens 1. I+R = 9months of Tx 2. I+R+Z (for the first 2 months) = 6months of Tx 3. COMMON PRACTICE (6months of Tx) a. Initial phase (1st 2months) i. I+R+Z+E/S 1. Eradication of mycobacterium 2. Conversion of +ve sputum to Spectrum of Activities –ve sputum b. Continuation phase (the last 1. Tuberculocidal for 4months) rapid growers i. I+R (extracellular) 1. Prevention of relapse 2. Tuberculostatic for 2. Complete mycobacterial slow growers eradication (intracellular) Prophylaxis (Preventive) Regimen 1. Daily dose of INH for 6 to12 months 2. Daily I+R doses for 6 months 3. If cant use INH a. Rifampicin 4months b. R+Z 2 months Side Effects 1. Peripheral Neuropathy a. INH promotes Pyridoxine (Vit B6) elimination b. Counter by VitB6 supplementation 2. Hepatotoxicity *Genetic polymorphism 1. Slow acetylator leads to ↑ susceptibility to toxicity Drug drug interaction 1. Potent CYP450 inhibitor Drugs/Infos Rifampicin Adsorption 1. Well absorbed orally Distribution 1. Readily distributed in all body fluid 2. Undergoes enterohepatic recycling 3. Easily reaches Tx level in CSF only during meningeal inflammation 4. Extensively bind to plasma protein Metabolism 1. Undergoes CYP450 metabolism Excretion 1. Urine 2. Bile Mechanism of Action 1. Binds to B subunit of bacterial DNAdependent RNA polymerase 2. Therefore inhibiting mRNA synthesis Spectrum of Activities 1. Bactericidal for a. Rapid growers b. Slow growers c. Spurters Side Effects 1. Common a. Rash b. Fever c. Arthralgia d. Nausea 2. Orange discoloration of a. Tears i. Permanently stained contact lens b. Sweats c. Urine 3. Hepatitis (rare) 4. High dose will lead to flu like syndrome Drug drug interaction 1. Potent CYP450 inducer 2. Should be replaced by less potent CYP450 inducer; Rifabutin in HIV patients undergoing HAART especially a. Protease inhibitor (Ritonavir) b. NNRTI (Efavirenz) Drugs/Infos Pyrazinamide Adsorption 1. Well absorbed orally Distribution 1. Readily distributed in all body fluid 2. Easily reaches Tx level in CSF only during meningeal inflammation Metabolism 1. Undergoes CYP450 metabolism Excretion 1. Urine Streptomycin Adsorption 1. Poorly absorbed orally 2. Given only parenterally Distribution 1. Poorly penetrates cellular membrane 2. Easily reaches Tx level in CSF only during meningeal inflammation Excretion 1. Urine in unchanged form Mechanism of Action Spectrum of Activities Side Effects 1. Active in acidic pH 1. Weak tuberculocidal to 2. Kill mycobacterium inside a. Intracellular the acidic lysosome mycobacterium 3. Converted to Pyrazinoic acid by Mycobacterial Pyrazinamidase 4. It is believed that it acts by inhibiting Fatty Acid Synthase at the Mitochondria and Cell membrane a. But still yet to be proven 1. Common a. Rash b. Fever c. Arthralgia d. Nausea 2. Hyperuriceamia a. May cause acute gouty attack 3. Hepatitis 1. It binds to the small 16S 1. Tuberculocidal only to rRNA of the 30S subunit of extracellular the bacterial ribosome mycobacterium 2. Interfering with the binding of formyl-methionyl-tRNA to the 30S subunit 3. Leading to codon misreading 1. Ototoxicity a. Hearing loss b. Vertigo 2. Nephrotoxicity Drugs/Infos Ethambutol Tuberculostatic Mechanism of Action Spectrum of Activities Ethambutol is an Arabinogalactan synthesis Adsorption inhibitor 1. Well absorbed orally 1. Inhibits the Distribution Mycobacterial 1. Poorly penetrates cellular Arabinosyl Transferase membrane 2. Therefore inhibiting the 2. Easily reaches Tx level in polymerization of CSF only during Arabinoglycan in cell meningeal inflammation wall synthesis Excretion 1. Urine in unchanged form 1. Tuberculostatic against rapid growers 2. Suppresses growth of most INH and streptomycin-resistant tubercle bacilli 3. Prevent emergence of resistance Side Effects 1. Optic neuritis a. Contraindicated in very small children to permit assessment of visual acuity and redgreen color discrimination