Anti mycobacterial drugs
advertisement

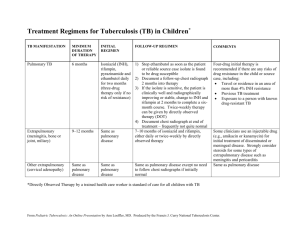
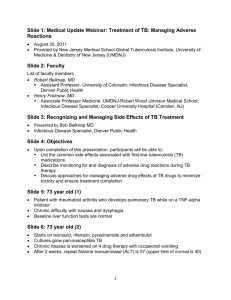
Antimycobacterial drugs By Bohlooli S, PhD School of Medicine, Ardabil University of Medical Sciences Drugs Used in Tuberculosis First Line Agents Isoniazid (INH) Rifampine Pyrazinamide Ethambutol Streptomycin Second Line Agents Amikacin Aminosalicylic acid Capreomycin Ciprofloxacin Clofazimine Cycloserine Ethionamide Levofloxacin Rifabutin Rifapentine Isoniazid (INH) Most active drug Water soluble Similar to pyridoxine Good penetration to phagocytic cells Isoniazid (INH): Mechanism of Action Prodrug: activated by KatG (Catalase proxidase) Active form bind to Acyl carrier protein (AcpM),and KasA (beta-ketoacyl carrier protein synthase), covalently Inhibits synthesis of mycolic acid Isoniazid (INH): Basis of Resistance Mutation or deletion of KatG Overexpression of inhA (encodes acyl carrier protein reducatase) Overexperssion of ahpC, oxidative stress protection Resistance mutants occur in 1 in 106 Isoniazid (INH): Pharmacokinetics Good absorption from GIT Readily distribute to tissues and body fluids Ratio in CFS: 20 to 100% Metabolism by N-acetyltransferase Rapid acetylator: hepatoxicity Slow acetylator: neuropathy Isoniazid (INH): Clinical Use Single agent in latent tuberculosis In combination with second agent in active form Use pyridoxine in conditions predisposing to neuropathy Isoniazid (INH): Adverse Reactions Allergic reactions Fever, skin rashes Drug induced systemic lupus erythematosus Direct toxicity Hepatitis: loss of appetite, nausea, vomiting, Jaundice, right upper quadrant pain In 1% patients and fatal Depend on age Neuropathy: higher in slow acetylators CNS effects: memory loss, psychosis, seizure Drug interaction: phenytoin Rifampin Active against: Mechanism: gram positive and gram negative cocci, some enteric bacteria Mycobacteria Chlamydia Binds to DNA dependent RNA polymerase Resistance: Point mutation in rpoB gene Prevent binding of rifampin to RNA polymerase Rifampin: Pharmacokinetic Well absorption Enterohepatic cycle Good distribution to body fluids and tissues and phagocytic cells Adequate level in meningeal inflammation Rifampin: Clinical use Together with other drugs for prevention of resistance Atypical mycobacterial infections Leprosy Alternative to INH Prophylaxis in H. influemzae type b contacts Staphylococcal infections highly penicillin-resistant strain of pneumococci Rifampin: adverse reactions Orange color urine, sweat, tears, contact lens Rashes, thrombocytopenia, nephritis Hepatitis Light chain proteinuria Flu-like syndrome: fever, chills, myalgias, anemia, thrombocytopenia, acute tubular necrosis Enzyme inducer Chemical Sructure Ethambutol Synthetic, water soluble, heat stable compound An inhibitor of arabinosyl transferase and polymerization of arabinoglycan Resistance due to mutations resulting in overexpression of emb gene products and occur rapidly Good absorption from GIT Elimination: 50% unchanged in Urine Ethambutol Clinical use In combination with isoniazid or rifampin Adverse reaction Retrobulbular neurotitis, loss of visual acuity, red green blindness Hypersensivity reactions Chemical Structure Pyrazinamide Relative of nicotinamide Inactive in neutral pH but active in acidic pH Drug taken up by macrophages Converted to pyrazinoic acid by bacterial pyrazinamidase Mechanism is unknown Clinical use: together with insoniazid or rifampin Resistance is fairly readily acquired Adverse reaction: hepatotoxicity, nausea, vomiting, drug fever, hyperuricemia Streptomycin Resistance is due to point mutation in gene rpsL, encoding S12 ribosomal protein or rrs, encoding 16S ribosomal rRNA Active against extracellular form of tubercle bacille Employed when injectable drug is needed Alternative second-line drugs for tuberculosis In the case of resistance to the drug of first choice In the case of failure of clinical response When expert guidance is available to deal with the toxic effects.