Histopathology procedures and standards
advertisement

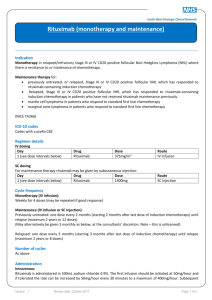
Indolent Lymphoma Haematological Pathway for South Wales Cancer Network Document Control Sheet Organisation Specialty/Project Document Title Document Number South Wales Cancer Network Haematological Site Specific Group Indolent Lymphoma Haematological Pathway 05/017 Version Author/s 1.0 Dr W Ingram Approved by South Wales Haematology Cancer Network Group Approval date Ratified by Dr W Ingram Dr C Fegan Date of next review TBC TBC South Wales Haematology Network Guidelines on the Diagnosis and Management of Indolent B-Cell Lymphomas Aims and Scope This guideline aims to cover general principles of the patient pathway for indolent lymphomas in Wales. The reader is directed to the excellent and comprehensive guidelines from the British Committee for Standards in Haematology (BCSH) for detailed guidelines on the management of specific disease entities. www.bcshguidelines.org.uk There are current BCSH guidelines for: Follicular lymphoma Mantle Cell lymphoma Waldenstrom’s Macroglobulinaemia Hairy Cell Leukaemia General Principles of Diagnosis and Staging Where possible, excision lymph node biopsy is preferable to core biopsy to ensure adequate tissue for diagnosis and to minimise delays. There should be agreed local pathways with surgeons to progress to rapid surgical biopsy in cases where radiology core biopsy is non-diagnostic. All cases should be discussed at a haematology MDT meeting: At diagnosis and on completion of staging, to confirm management plan and discuss any relevant clinical trials At review of interim and post-treatment imaging, to decide on appropriate management. Histopathology procedures and standards Each MDT meeting should have at least one designated Pathologist from the All Wales Lymphoma Panel (AWLP) who will review material from all new lymphoma diagnoses. All lymphomas are to be reported according to the WHO classification system and should include relevant prognostic biomarkers where possible. For the majority of cases a preliminary source report should be available within 5 working days of receiving the specimen and an AWLP report should be available within 10 working days. More complex cases, and those requiring extensive immunohistochemistry and/or molecular analysis will take longer to report. Production of an interim report recommended in such cases. Staging and pre-treatment investigations Clinical history including any history of immunosuppression Documentation of presence or absence of systemic symptoms Clinical examination ECOG Performance status is Calculation of relevant prognostic score where available eg MIPI, FLIPI2 FBC and blood film, liver and renal function, LDH, bone profile, immunoglobulins, beta-2 microglobulin and protein electrophoresis HIV, HBsAg, HBcAb and HBsAb and Hep C Ab testing Contrast enhanced CT Neck/chest/abdomen/pelvis Bone marrow examination (aspirate and trephine) Immunophenotyping of peripheral blood or bone marrow or lymph node biopsy material, when appropriate FDG-PET is of uncertain value in low grade lymphomas. Routine use should be considered only in the setting of a clinical trial In addition to staging the head and neck, MRI is the diagnostic procedure of choice for rare patients with suspected disease in the CNS disease including brain, leptomeninges and spinal cord An echocardiogram and ECG should be performed for all patients being considered for anthracycline based therapy who are over the age of 70 years or who have cardiac risk factors. Pregnancy testing in females of child bearing age prior to any chemotherapy. Fertility preservation All men should be offered the option for sperm storage All women of childbearing potential should be offered the option for egg collection and storage prior to starting chemotherapy. However, the following should be noted 1. CHOP based chemotherapy is unlikely to be sterilising 2. Egg collection will delay treatment starting by approximately 1 month Patients who are unwell from their lymphoma are unlikely to get a good egg harvest and should get on with treatment urgently Information Required at MDT Clinical summary, ECOG performance status Final staging Named key worker WHO/ICD diagnostic code Specific Disease Entities; special considerations Follicular lymphoma Covered in separate, detailed document Mantle Cell Lymphoma In addition to routine staging tests, consider imaging of GI tract, if there are gastrointestinal symptoms Similarly, while not recommended routinely, diagnostic lumbar puncture should be considered in those with symptoms suggestive of central nervous system (CNS) disease Use of Rituximab containing regimes is recommended in BCSH Guideline 2012, but there is no NICE guidance. Some Health Boards are requiring IPFR application. Recommended first line treatment Young/fit (under 65y): Nordic chemotherapy protocol (alternating R-maxiCHOP/R-Cytarabine), followed by consolidation with BEAM autograft. Older/less fit: Options include Fludarabine, Cyclophosphamide, Rituximab (FCR), RCHOP for the fairly fit, Chlorambucil +Rituximab (elderly,frail, comorbidities) Clinically indolent disease: A subset of patients, often those with splenomegaly, but little nodal disease, appear to have a clinically indolent course, and initial watch and wait may be appropriate. Early stage disease, outside a clinical trial, consider radiotherapy Waldenstrom’s Macroglobulinaemia Diagnosis, Staging and Monitoring To avoid difficulties of interpretation, sequential IgM monitoring should be performed in a single laboratory using a single methodology The value of SFLC ratio has not been established in WM, and should not be used routinely Tissue biopsy is recommended in patients suspected of histological transformation In patients with neuropathy, check anti-MAG antibodies Treatment BCSH Guideline (2014) recommends that symptomatic patients, requiring therapy, should receive a Rituximab containing regime. Appropriate regimes include dexamethasone, rituximab, cyclophosphamide (DRC), bendamustine, rituximab (BR). Fludarabine, rituximab (FR), fludarabine, cyclophosphamide, rituximab (FCR) and cladribine,rituximab (clad-R). As for Mantle Cell Lymphoma, in some Health Boards in Wales, this will necessitate IPFR, there being no NICE guidance in WM. Given the risk of IgM flare, careful monitoring of all patients receiving Rituximab is required RCHOP should not be used as primary therapy in WM Chlorambucil remains suitable therapy in elderly, frail patients Bortezomib is not recommended for 1st line therapy, outside a clinical trial IgM associated neuropathy Joint care with a Neurologist recommended Consider treatment (with a Rituximab containing regime) in patients with rapidly progressive or disabling anti-MAG neuropathy Hyperviscosity Syndrome Plasma exchange:1-2 procedures, 1-1.5 plasma volume recommended Hairy Cell Leukaemia Key points Purine analogues, cladribine or pentostatin are recommended first line treatments Aim for complete remission, giving a second cycle of cladribine or pentostatin if necessary Addition of Rituximab recommended for relapsed or refractory disease Interferon alpha can be useful initial treatment in patients with severe pancytopenia Hairy Cell Variant responds poorly to purine analogues, and if treatment is required, splenectomy is probably the treatment of choice, but there is inadequate data to make firm recommendations.