Rituximab - TTP Network
advertisement

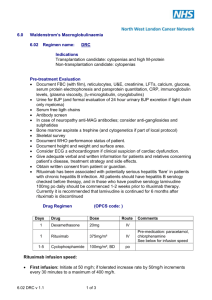
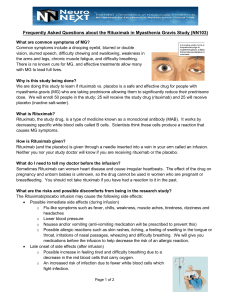
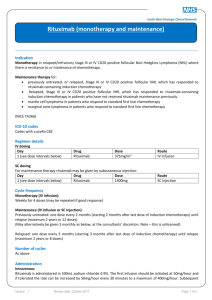
Rituximab Information Leaflet for Thrombotic Thrombocytopenia Purpura (TTP) patients You have been prescribed Rituximab to treat your TTP. Rituximab is a monoclonal antibody. It works by recognising the protein (CD20) on the surface of one of the main types of normal white blood cells (B-cell lymphocytes) and then binding onto it (like a key in a lock) and remove the cells producing the antibodies causing TTP. Rituximab is given during the acute TTP episode when you are in hospital, and can also be given in the out-patient setting if your enzyme level: ADAMTS13 is lowered from previous stable readings. Before Rituximab is administered, we will check your Hepatitis status. Depending on the results, you may be started on a drug called Lamivudine. How is it given? Rituximab is clear colourless fluid after being diluted. It is given as a drip (infusion) through a fine tube (cannula) inserted into a vein. The first infusion is usually given slowly eg over 8-12 hours when you are an in-patient. This is because it is not uncommon to get a reaction with the first infusion, associated with shivering, temperature, shaking. This is an allergic reaction. The nurses looking after you are very familiar with Rituximab and will slow/stop the infusion temporarily and give you further medication to reduce the symptoms. One of these medications, Piriton, is anti-histamine and can make you very sleepy. Subsequent infusions (depending on degree of reaction experienced) will be administered over 2-4 hours. Timing of administration will be determined by your consultant. You may have anything between 4 and 8 Rituximab infusions when you present with TTP. Longer term we monitor you in the outpatients ‘clinic and if your ADAMTS 13 drops to low levels, even though you are well, we will give you further Rituximab to prevent you having a TTP relapse. Possible reactions / side effects Everyone reacts differently to Rituximab. Some people have very few side effects, while others may experience more. Side effects are generally mild and can be reduced with medicines. Listed below are the most common side effects: Flu-like symptoms: these can include a high temperature, chills, weakness, muscle aches, tiredness, dizziness and headaches. They can occur while the Rituximab is being given, but do not usually last long. Low blood pressure: this may happen during the infusion, so your blood pressure readings will be checked regularly during the infusion. Feeling sick and occasional vomiting: you will be given anti-sickness tablets. If you find the sick feeling persists, please inform the nurse who will get a stronger anti-sickness medication prescribed for you. Allergic reactions: you may have a slight allergic reaction to the Rituximab. Signs of this include skin rashes and itching, a feeling of swelling in the tongue, irritation of the nasal passages, wheezing, a cough and breathlessness. You are monitored closely throughout the infusion, but if you experience any of these symptoms, please let the nurses know. Lowered resistance to infection: Rituximab can reduce the production of antibodies making you more prone to infection. Lowered White Blood Cells: occasionally neutropenia can be seen post administration of Rituximab. Flushing: you may experience sudden warmth in your face as well as some redness or darkening. This can happen for a short time during the infusion. Joint pains: very occasionally patients can complain of joint pains, especially in the knees. PML: Progressive multifocal leukoencephalopathy is a rare viral disease of the brain. It is associated with certain immunosuppressive or immunomodulatory therapies. What conditions is Rituximab used in as a treatment If you look up Rituximab on the internet, you will see it is primarily used in a type of blood cancer called lymphoma. But it is also licensed for use in an autoimmune condition called rheumatoid arthritis. Rituximab is not licensed in TTP, but is shown to be very effective in getting patients into remission and preventing relapse. It is also used in other haematological conditions that are not blood cancers that are due to the immune system being unregulated. Contact Names / Numbers for the TTP Team TTP Lead Consultant: Dr Marie Scully TTP Consultant: Dr John –Paul Westwood TTP Data Manager: Debra Elllis TTP Clinical Nurse Specialist: Siobhan Mc Guckin: 07908 175363 Out of Hours / Urgent Medical Advice Number: 07852 220900 Approved By: Dr Marie Scully, Dr JP Westwood and Siobhan Mc Guckin