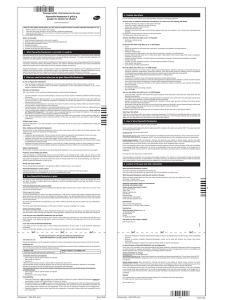
NCH Sepsis ED EGDT Orders - Hospital Council of Northern and
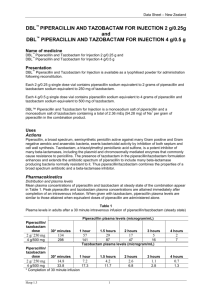
advertisement
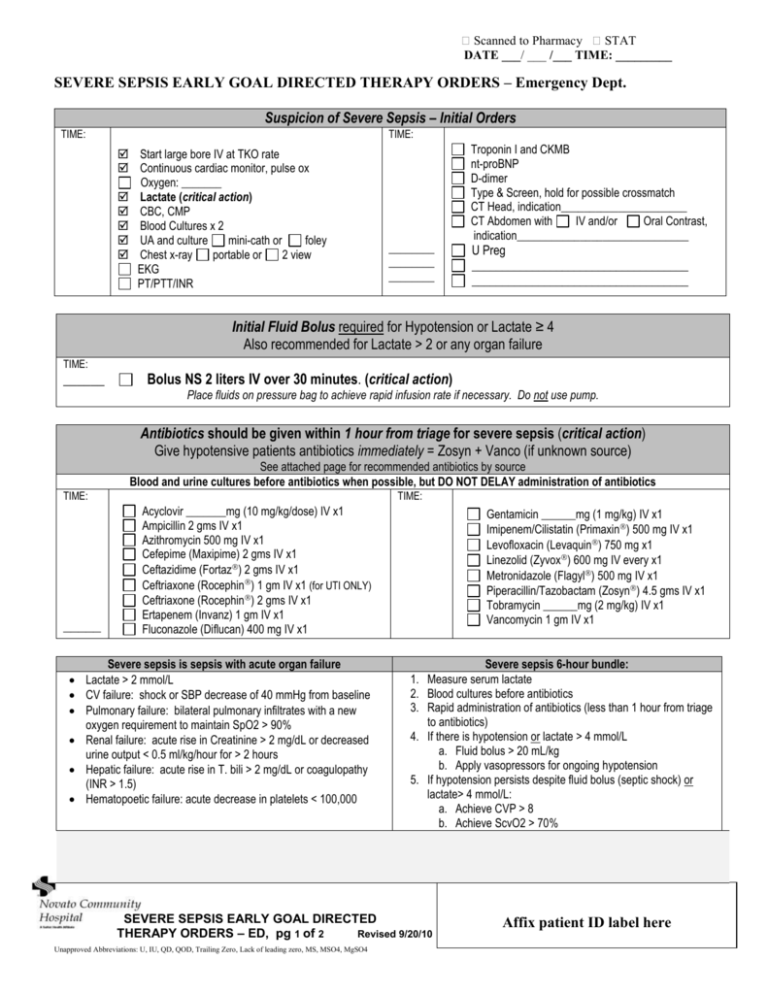
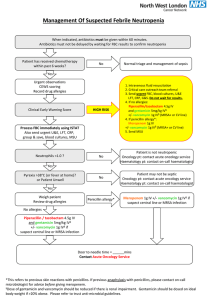
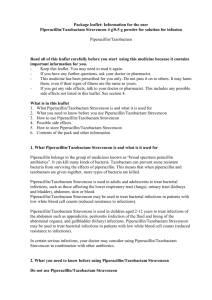
� Scanned to Pharmacy � STAT DATE ___/ ___ /___ TIME: _________ SEVERE SEPSIS EARLY GOAL DIRECTED THERAPY ORDERS – Emergency Dept. Suspicion of Severe Sepsis – Initial Orders TIME: TIME: Start large bore IV at TKO rate Continuous cardiac monitor, pulse ox Oxygen: _______ Lactate (critical action) CBC, CMP Blood Cultures x 2 UA and culture mini-cath or foley Chest x-ray portable or 2 view EKG PT/PTT/INR ________ ________ ________ Troponin I and CKMB nt-proBNP D-dimer Type & Screen, hold for possible crossmatch CT Head, indication______________________ CT Abdomen with IV and/or Oral Contrast, indication______________________________ U Preg ____________________________________ ____________________________________ Initial Fluid Bolus required for Hypotension or Lactate ≥ 4 Also recommended for Lactate > 2 or any organ failure TIME: ______ Bolus NS 2 liters IV over 30 minutes. (critical action) Place fluids on pressure bag to achieve rapid infusion rate if necessary. Do not use pump. Antibiotics should be given within 1 hour from triage for severe sepsis (critical action) Give hypotensive patients antibiotics immediately = Zosyn + Vanco (if unknown source) See attached page for recommended antibiotics by source Blood and urine cultures before antibiotics when possible, but DO NOT DELAY administration of antibiotics TIME: _____ TIME: Acyclovir _______mg (10 mg/kg/dose) IV x1 Ampicillin 2 gms IV x1 Azithromycin 500 mg IV x1 Cefepime (Maxipime) 2 gms IV x1 Ceftazidime (Fortaz) 2 gms IV x1 Ceftriaxone (Rocephin) 1 gm IV x1 (for UTI ONLY) Ceftriaxone (Rocephin) 2 gms IV x1 Ertapenem (Invanz) 1 gm IV x1 Fluconazole (Diflucan) 400 mg IV x1 Severe sepsis is sepsis with acute organ failure Lactate > 2 mmol/L CV failure: shock or SBP decrease of 40 mmHg from baseline Pulmonary failure: bilateral pulmonary infiltrates with a new oxygen requirement to maintain SpO2 > 90% Renal failure: acute rise in Creatinine > 2 mg/dL or decreased urine output < 0.5 ml/kg/hour for > 2 hours Hepatic failure: acute rise in T. bili > 2 mg/dL or coagulopathy (INR > 1.5) Hematopoetic failure: acute decrease in platelets < 100,000 Gentamicin ______mg (1 mg/kg) IV x1 Imipenem/Cilistatin (Primaxin) 500 mg IV x1 Levofloxacin (Levaquin) 750 mg x1 Linezolid (Zyvox) 600 mg IV every x1 Metronidazole (Flagyl) 500 mg IV x1 Piperacillin/Tazobactam (Zosyn) 4.5 gms IV x1 Tobramycin ______mg (2 mg/kg) IV x1 Vancomycin 1 gm IV x1 Severe sepsis 6-hour bundle: 1. Measure serum lactate 2. Blood cultures before antibiotics 3. Rapid administration of antibiotics (less than 1 hour from triage to antibiotics) 4. If there is hypotension or lactate > 4 mmol/L a. Fluid bolus > 20 mL/kg b. Apply vasopressors for ongoing hypotension 5. If hypotension persists despite fluid bolus (septic shock) or lactate> 4 mmol/L: a. Achieve CVP > 8 b. Achieve ScvO2 > 70% SEVERE SEPSIS EARLY GOAL DIRECTED THERAPY ORDERS – ED, pg 1 of 2 Revised 9/20/10 Unapproved Abbreviations: U, IU, QD, QOD, Trailing Zero, Lack of leading zero, MS, MSO4, MgSO4 Affix patient ID label here � Scanned to Pharmacy � STAT DATE ___/ ___ /___ TIME: _________ SEVERE SEPSIS EARLY GOAL DIRECTED THERAPY ORDERS – Emergency Dept. For Lactate ≥ 4 or Septic Shock (hypotension unresponsive to Initial Fluid Bolus), begin Early Goal Directed Therapy Critical Actions 1) Place central line (in superior vena cava) 2) Achieve CVP ≥ 8 3) Achieve MAP ≥ 65 4) Achieve ScvO2 ≥ 70 Achieve all goals in less than 6 hours TIME: Consent for Central Line placement, set up for Edwards Catheter placement Monitor CVP continuously, record every 30 minutes Monitor ScvO2 continuously, record every 30 minutes Fluids (CVP goal ≥ 8) CVP Measurement <8 (<12 for ventilated 8-12 (12-15 for ventilated) >12 (>15 for ventilated) Vasopressors (MAP goal ≥65) TIME: Action Bolus NS 1000 ml every 30 minutes until CVP >8 Maintenance fluids: NS 250 ml/hr, OR __________ml/hr IV to TKO (15 ml/hr) Initiate Pressors immediately after initial fluid bolus if MAP remains <65 TIME: NORepinephrine (Levophed) 4mg in 250 ml D5W (16 mcg/ml) IV drip Start at 4 mcg/min, titrate 2 mcg/min every 10 minutes to achieve MAP ≥65 (Maximum rate = 20 mcg/min, notify MD if at maximum and MAP <65) DOPamine 400 mg in 250 ml D5W (1600 mcg/ml) IV drip Start at 5 mcg/kg/min, titrate 2.5 mcg/min every 10 minutes to achieve MAP ≥65. (Maximum rate = 20 mcg/kg/min, notify MD if at maximum and MAP <65) Transfusion (ScvO2 goal ≥70%) TIME: OR Once CVP and MAP goals are met, if ScvO2 <70% transfuse pRBC until goal Hgb ≥10 TIME: TRANSFUSE ___ unit(s) pRBC(s), each unit over 1 hour. Draw stat hemogram one hour after last unit (Use Transfusion Order Set) Inotrope (ScvO2 goal ≥70%) Once CVP and MAP goals are met and Hgb ≥10, if ScvO2 <70% initiate DOBUTamine DOBUTamine 500 mg in 250 ml D5W (2000mcg/ml) IV drip Start at 2.5 mcg/kg/min, titrate 2.5 mcg/kg/min every 10 minutes to achieve ScvO2 ≥70% (Maximum Rate 20 mcg/kg/min) (Notify MD for MAP >75 or HR >120) TIME: TIME: Repeat Lactate, 6 hours after triage time Prescriber’s Name (PRINTED) MD ID# Prescriber’s Signature Date Time RN’s Signature Date Time SEVERE SEPSIS EARLY GOAL DIRECTED THERAPY ORDERS – ED, pg 2 of 2 Revised 9/20/10 Unapproved Abbreviations: U, IU, QD, QOD, Trailing Zero, Lack of leading zero, MS, MSO4, MgSO4 (pref.) Pager # (pref.): Affix patient ID label here ANTIBIOTICS RECOMMENDATIONS Hospital Acquired or Healthcare Associated (HIGH RISK for Resistant Pathogens) Community Acquired (LOW RISK for Resistant Pathogens) Suspected Source of Infection SKIN/SOFT TISSUE UNCOMPLICATED VANCOMYCIN + CEFTRIAXONE VANCOMYCIN AND (choose one) SKIN/SOFT TISSUE- COMPLICATED (NECROTIZING FASCITIS, DM FOOT) VANCOMYCIN AND (choose one) PIPERACILLIN/TAZOBACTAM OR LEVOFLOXACIN + METRONIDAZOLE PNEUMONIA REFER TO PNEUMONIA ORDER SET PSEUDOMONAS RISK=(bronchiectasis OR structural lung disease such as COPD, restrictive or interstitial lung disease, pulmonary fibrosis, chronic bronchitis, emphysema AND repeated antibiotic or steroid courses in past year) URINARY TRACT PIPERACILLIN/TAZOBACTAM OR LEVOFLOXACIN + METRONIDAZOLE NO PSEUDOMONAS RISK: CEFTRIAXONE AND AZITHROMYCIN PSEUDOMONAS RISK: PIPERACILLIN/TAZOBACTAM + LEVOFLOXACIN OR CEFEPIME + LEVOFLOXACIN IF MRSA risk ADD VANCOMYCIN OR LINEZOLID CEFTRIAXONE *HCAP…includes VAP VANCOMYCIN OR LINEZOLID PLUS (choose one) PIPERACILLIN/TAZOBACTAM OR CEFTAZIDIME PLUS (choose one) LEVOFLOXACIN OR TOBRAMYCIN PIPERACILLIN/TAZOBACTAM OR CEFTAZIDIME + GENTAMICIN OR INTRA-ABDOMINAL PIPERACILLIN/TAZOBACTAM LEVOFLOXACIN + GENTAMICIN PIPERACILLIN/TAZOBACTAM OR LINE SEPSIS ENDOCARDITIS VANCOMYCIN + CEFTRIAXONE MENINGITIS CEFTRIAXONE + VANCOMCYIN Age > 50 ADD AMPICILLIN UNKNOWN SOURCE VANCOMYCIN + PIPERACILLIN/TAZOBACTAM ERTAPENEM VANCOMYCIN AND PIPERACILLIN/TAZOBACTAM VANCOMYCIN + PIPERACILLIN/TAZOBACTAM + GENTAMICIN STRONGLY recommend ID consult VANCOMYCIN + CEFTAZIDIME Age> 50 ADD AMPICILLIN STRONGLY recommend ID consult SEVERE PENICILLIN ALLERGY VANCOMYCIN + PIPERACILLIN/TAZOBACTAM AND TOBRAMYCIN LEVOFLOXACIN + VANCOMYCIN + TOBRAMYCIN *Healthcare-associated pneumonia (HCAP) is defined as pneumonia that occurs in a non-hospitalized patient with extensive healthcare contact, as defined by one or more of the following: - Intravenous therapy, wound care, or intravenous chemotherapy within the prior 30 days - Residence in a nursing home or other long-term care facility - Hospitalization in an acute care hospital for two or more days within the prior 90 days - Attendance at a hospital or hemodialysis clinic within the prior 30 days ***THIS PAGE FOR REFERENCE ONLY*** Severe Sepsis Early Goal Directed Therapy Orders Emergency Department page 3 of 3 Revised 9/20/10