Sepsis - CriticalCareMedicine
advertisement
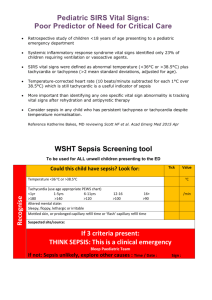
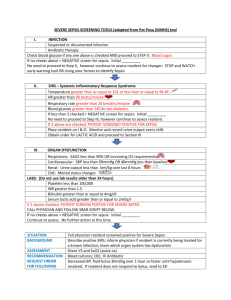
Sepsis 54 year old man with a past history of smoking and diabetes presents to the emergency department with a one week history of progressive unwellness. He describes fever and chills over the last three days with cough and swelling around his left ankle. At the triage desk, his blood pressure is 83/44, heart rate 105, and oxygen saturations 87% Does this patient have sepsis? What is the definition of SIRS, sepsis, severe sepsis, and septic shock? SIRS – Two or more of the following: – Temperature >38.5 or <35.0 – Heart rate >90 – Respiratory rate >20 or PaCO2 <32 – WBC >12 or <4 or >10% bands Sepsis – SIRS in response to documented infection Severe Sepsis – Sepsis and at least one of the following signs of organ hypoperfusion or dysfunction: – – – – – – – – – Mottled skin Capillary refill > 3 seconds Urine output < 0.5 mL/kg for at least one hour Lactate > 2 mmol/L Change in mental status Platelet count < 100 DIC ARDS Cardiac dysfunction on echocardiogram Septic Shock – Severe sepsis and MAP < 60 mmHg and need for vasopressors After bringing the patient into the acute care area of the ER, he appears more tachypneic and confused. What should you do next? After starting flush oxygen and inserting two IVs, the patient continues to be confused, hypotensive, tachycardic and tachypneic. Initial ABG: pH 7.21, PCO2 27, PO2 95, HCO3 14, lactate 5.2 WBC 19.3, Bands 21% Creatinine 213, Urea 17.3 This patient meets the criteria for sepsis. What are the possible sources? What should be done within the next hour? Why is source control and early antibiotics critical in sepsis? After securing the airway, inserting a central line and arterial line, starting antibiotics and sending cultures, the patient’s CVP is 4. Is this a problem and what should be done? After giving 2 litres of normal saline, the CVP is 10 but the MAP is 60 mmHg. Is this acceptable and what should be done about it? Levophed is started and titrated to a goal of 65 mmHg. The central venous saturations are now 56%. What would you do next? What is the pathophysiological relationship between inflammation and complement activation, coagulation, and antifibinolysis? What adjunct treatments can be used in sepsis to modulate the inflammatory system? What is the role of other supportive therapies such as steroids, vasopressin, and insulin? Questions??