What`s New in the ICU? The Top Five New
advertisement

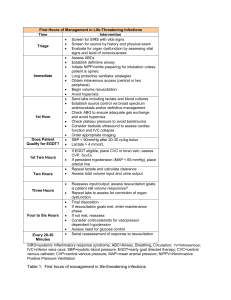
Goal-Directed Therapy in Septic Shock What Goals Matter, What Don’t, and Why We Should Care William Owens, MD Division of Pulmonary and Critical Care Medicine University of South Carolina Disclosures I have no ties, financial or otherwise, with any companies or products discussed today. I do have biases, prejudices, and opinions completely unfounded in fact, which I am always happy to share! Patients enrolled who had either: SBP < 90 after a 20 mL/kg fluid bolus, or Lactate > 4 mmol/L 46% vs 30% INTERVENTION ARM Early Antibiotics Fluid Resuscitation Good Genetics CVP 8-12 Hemoglobin 10 g/dL ScvO2 ≥ 70% GOAL: Fill The Tank! Pulmonary Artery Catheter Central Venous Pressure AUC 0.56 Measurement CVP< 8 CVP< 12 CVP< 5 PAOP< 11 PAOP< 11 + CVP< 8 CVP< 8 + SVI< 30 PAOP< 12 + SVI< 30 PPV 51% 47% 47% 54% 54% 61% 69% NPV 65% 67% 58% 74% 63% 39% 58% (PPmax – PPmin) (PPmax + PPmin/2) PPV≥13% correlates with preload responsiveness (AUC 0.91) * Tidal Volume should be 8 cc/kg * Breathing should be controlled and passive * Cardiac rhythm must be regular 12% change corresponds with fluid responsiveness PPV 93% NPV 92% Feissel M, Michard F, Faller J, Teboul J The respiratory variation in inferior vena cava diameter as a guide to fluid therapy Intensive Care Med (2004) 30: 1834-1837 LVEDA < 10 cm2 or LVEDA/BSA < 5.5 cm2/m2 corresponds with preload responsiveness GOAL: Fill The Tank! CVP is not accurate at any level The PA catheter isn’t much better Ultrasound and PPV show promise Clinical Correlation Is Required! GOAL: Hemoglobin ≥ 10 g/dL CaO2 = 1.34 × Hgb × SaO2 DO2 = CO × CaO2 × 10 838 patients randomized Transfusion triggers of 7.0-9.0 g/dL versus 10.0-12.0 g/dL No difference in mortality overall Shock Drop in Hgb > 3 g/dL NoCoronary differenceIschemia in mortality in patients with coronary artery disease Not Applicable to Initial Resuscitation? Inadequate Oxygen Delivery Benefits Outweigh Risks Transfusion Increases DO2 and VO2 Cells Can Use Delivered Oxygen Inadequate Oxygen Delivery Healthy humans can tolerate hemodilution to 5 g/dL DO2crit in animals seems to be 3-3.5 g/dL Microcirculatory hematocrit is relatively constant at 12-15% No necrosis at autopsy Transfusion Increases DO2 and VO2 Mathematical Coupling Stored Blood Holds On To Oxygen Supply Dependency Doesn’t Exist In Septic Shock Cells Can Use Delivered Oxygen RBCs are depleted of 2-3 DPG until 24 hours after transfusion Free Hemoglobin scavenges NO— inflammation, vasoconstriction, thrombosis, oxidative stress Increasing blood viscosity causes vasodilation via endothelium-released NO (much of the benefit of transfusion may be independent of CaO2) Marik showed that patients transfused stored blood had consistently lower gastric mucosal pH (JAMA 1993;269(23):3024– 9) 80% 95% GOAL: Hemoglobin ≥ 10 g/dL No evidence for arbitrary transfusion trigger Transfused RBCs may worsen microcirculatory perfusion Base decision to transfuse on signs of inadequate oxygen delivery • • • • Rising lactate Elevated troponin Ischemic ECG findings Poor perfusion (i.e., the cold big toe) GOAL: Keep ScvO2 ≥ 70% VO2 = CO × 1.34 × Hgb × [SaO2 –SvO2] Shoemaker (Chest, 1988) • Get CI over 4.5 L/min/m2 • DO2I >600 mL/min/m2 • VO2I >170 mL/min/m2 Tuchschmidt (Chest, 1992) • Supranormal DO2 in Septic Shock • No Survival Benefit Gattinoni (NEJM, 1995) • CI >4.5 L/min/m2 • SvO2 >70% • No Survival Benefit • Many patients couldn’t reach physiologic targets Nguyen et al: ED Resuscitation Improves Survival (Acad Emerg Med, 2000) PRO • Low ScvO2 is useful for titrating inotropes in cardiogenic shock • A low admission ScvO2 may predict higher mortality CON • Global measurement of oxygen delivery • Transfusion of RBCs raises ScvO2 but doesn’t improve sublingual microcirculatory flow • May be elevated due to pathologic shunting • Septic shock is due to cellular dysoxia, not hypoxia Sources of Lactic Acid in Septic Shock Anaerobic Metabolism (bowel/hepatic ischemia) Acute Lung Injury/ARDS Dysfunctional Cellular Metabolism • Inactivation of Pyruvate Dehydrogenase • NO suppression of mitochondrial respiration • Excessive pyruvate production due to catecholamines ICU Mortality and Time to Lactate Clearance (< 2 mmol/L) 42.50% 45.00% 40.00% 35.00% 30.00% Lactate Clearance: A Better Goal Than ScvO2? 25.00% 20.00% 15.00% 10.00% 5.00% 0.00% 3.90% Less than 24 hours More than 48 hours Am J Surg 2001;182(5):481-5 Fill the Tank, but Forget the Filling Pressures Bedside Ultrasound and Pulse Pressure Variation are superior to CVP and PAOP for guiding fluid resuscitation Preload Responsiveness Doesn’t Always Mean The Patient Needs Volume “Warm around the edges” is a good rule to follow Transfuse Sparingly and Selectively A hemoglobin >7 g/dL is usually OK Raising the hematocrit may raise the SvO2, but not necessarily tissue perfusion Your attendings were right—treat the patient, not the number Markers of Dysoxia Are Better Than Markers of Hypoxia Septic shock is not a low-flow, low-oxygen disease Early aggressive resuscitation is key Babies may be big at Baptist, but lactate is also for the ICU Division of Pulmonary, Critical Care, and Sleep Medicine wowens@uscmed.sc.edu