A Vitamin T Overdose? : An audit of piperacillin/ tazobactam use at
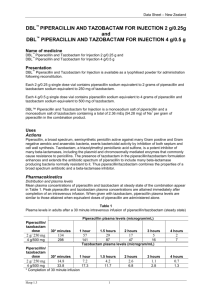
advertisement
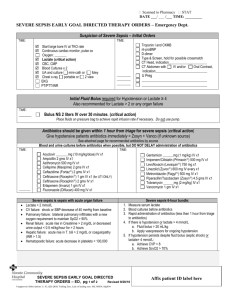
+ A Vitamin T Overdose? : An audit of piperacillin/ tazobactam use at Royal Perth Hospital Amelia Davis and Matthew Hanson Contributors: Dr Susan Benson, Dr Owen Robinson, Matthew Rawlins + Background Piperacillin/ tazobactam (commonly: Tazocin) 4g + 0.5g tds B lactam + B lactamase inhibitor Broad spectrum: gram positive, gram negative* and anaerobes* Largely replaced ticarcillin/clavulanate (Timentin) in 2010 “Unrestricted” + Introduction Restrictions for other antibiotics: Broad spectrum cephalosporins Carbapenems Glycopeptides Flouroquinolones Others Lack of specific guidelines or restrictions for piperacillin/ tazobactam + Purpose Review the indications and appropriateness of piperacillin/ tazobactam Attempt to highlight hospital specific factors influencing prescribing + Methods A cross sectional, point prevalence study National Antimicrobial Prescribing Survey 571 inpatients at Royal Perth Hospital on 14/11/12 To quantify and analyse the use of antimicrobials Identified patients on piperacillin/ tazobactam (n=78) Recalled patient notes Recorded indication for antibiotic, diagnosis, frequency of administration and prescribing department All non-concordant prescriptions reviewed by two ID Physicians + Methods Category C- Concordant with guidelines NC(A)- Non- concordant with guidelines but deemed Appropriate by ID review NC (IA) – Non- concordant with guidelines (Inappropriate choice) F- Correct Choice but incorrect frequency Where C= Concordant with therapeutic guidelines or RPH guidelines + Results Overall Category Number of Patients (n=78) C- Concordant with guidelines 25 (32%) NC(A)- Non- concordant with guidelines but deemed Appropriate by ID review 19 (24%) NC (IA) – Non- concordant with guidelines (Inappropriate choice) 34 (44%) F- Correct Choice but incorrect frequency 4 (5%) + Results Category C – Concordant with guidelines Indication Peritonitis Diabetic Ulcer Contaminated Wound Animal/Human Bite Aspiration Pneumonia HAP – high risk Febrile Neutropaenia Necrotising Pancreatitis Number (n=25) 9 4 3 3 3 1 1 1 + Results Category NC(A) – Not concordant with guidelines but deemed an appropriate choice by ID Physicians Indication Abdominal infections Skin infections Respiratory infections Urinary tract infections Abdominal infections included: • appendicitis • cholecystitis • abscess • fistulae • bowel necrosis • non-specific infective surgical abdomen Number (n=19) 12 3 2 2 + Results Category NC(IA) – Not concordant with guidelines – inappropriate choice Indication Poor antibiotic reasoning (47%) No indication for antibiotic “Febrile Neutropaenia” (not meeting criteria for neutropaenia) Prolonged post-surgical prophylaxis Unnecessary broad CAP spectrum of action Empirical UTI (53%) Cellulitis Wound infection – without systemic symptoms Number (n=34) 11 3 2 6 4 2 2 + Breakdown by department Appropriate Not Appropriate Medical 12 20 Surgical 32 14 Chi- squared test P= 0.0049 Statistically significant difference between medical and surgical teams + Frequency/Dose Frequency 3 incidences of bi- daily dosing 1 incidence of alternate day dosing All documented to be due to “renal impairment” None actually met criteria for reduced dosing (GFR <20ml/min) Dosing All 78 prescriptions 4 + 0.5g + Limitations Cross sectional, retrospective study Sample size Poor documentation Did not formally analyse duration of therapy + Conclusions What we do well Piperacillin/ tazobactam was appropriate in 56% Common appropriate indications: Peritonitis Diabetic ulcers What we don’t do so well Piperacillin/ tazobactam was inappropriate in 44% Poor antibiotic reasoning Unnecessary use of broad spectrum Documentation + Further Questions Raised? Why are we prescribing inappropriately? Over treating? Medical vs Surgical? Restricted use of other antibiotics? Concern about risk of toxicity with aminoglycosides use? What do we do now? Education re: common inappropriate uses Improve documentation + Questions?