RESPIRATORY SYSTEM
advertisement

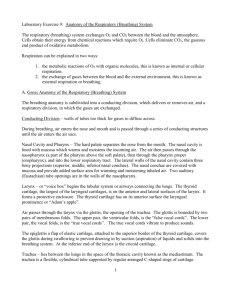
RESPIRATORY SYSTEM 1. 1. 1. Introduction 1. General function 1. 1. provide a specialized surface for the efficient exchange of respiratory gases 2. 2. pulmonary ventilation - movement of air between external environment and air sacs 3. 3. external respiration - diffusion of gas molecules between air sacs and capillaries 4. 4. internal respiration - diffusion of gases between blood cells and body cells 5. 5. what we call respiration is 2, 3,and 4 together, not cellular respiration 2. 2. 1. Organs of Respiration 1. Divisions 1. 1. based on location: upper respiratory tract (head and neck) and lower r.t. (thoracic cavity) 2. 2. based on function: conduction zone (organs that move air) and respiratory zone (where gas exchange takes place) 2. Nose 1. 1. external nares divided by nasal septum which opens into a vestibule (chamber) which opens into larger nasal cavity 1. 1. nasal cavity divided by 3 conchae which increase surface area 2. 2. paranasal sinuses - cavities in skull associated w/ nasal cavity via narrow ducts which clog during infection 3. 3. functions of the nose 1. 1. warm air - mucous membrane w/ blood vessels 2. 2. humidify air - mucous membrane 3. 3. filter large particles - m.m. cilia and hairs 2. 3. 3. 1. 2. 4. 4. 1. 2. 5. 3. 5. 1. 2. 3. 4. Pharynx 1. throat that extends from nasal cavity to larynx 1. 1. walls of skeletal muscle lined by mucous membrane 2. divided into 3 segments 1. 1. nasopharynx - superior portion 2. 2. oropharynx and laryngopharynx - common passageway for air and food Larynx 1. connects pharynx to trachea 1. 1. lined by cartilage rings, some form Adam's apple 2. 2. lined by cilia that sweep mucus upward 3. 3. glottis - opening into larynx, 2. epiglottis prevents food from entering trachea by covering glottis during swallowing 3. contains vocal cords where sound is produced Trachea 1. tube surrounded by smooth muscle, cartilage, and elastic fibers 2. 12 cm long connecting larynx w/ bronchi 3. cartilage rings in the shape of a C, prevent trachea from collapsing when food is passing in the posterior esophagus 4. lined w/ pseudosratified ciliated columnar epithelium (PSCC) which 6. 6. 1. 2. 3. 7. 7. 1. 2. 3. 4. 3. 3. 1. secretes mucus to trap foreign particles, cilia beat in unison to move trapped particles to back of throat where they are swallowed or expelled Bronchial Tree 1. primary bronchi - split at distal end of trachea into 2 bronchi 1. 1. left branches at greater angle, most foreign materials end up in right bronchi 2. bronchial tree - further branches as bronchi enter lungs, smaller and narrower, cartilage disappears and mucous membrane becomes thinner 1. 1. bronchioles - small tubes lined by elastic tissue and smooth muscle 2. 2. alveolar ducts - further division of bronchioles 3. alveoli - 300-500 million in lungs of normal adult 1. 1. terminal point of respiratory system 2. 2. only site of gas exchange between external environ. and blood 3. 3. surface area of a tennis court (70m2) 4. 4. thin wall of squamous epithelium separates alveoli from capillaries 5. 5. surfactant - detergent like lipid molecules lining inner surface of alveoli, necessary for gas exchange and to overcome surface tension created as alveoli collapse during expiration; not present in preemies 6. 6. respiratory membrane - alveoli plus capillaries Lungs 1. site of gas exchange between atmosphere and blood 2. consist of bronchial tree, alveoli, capillary network and supporting tissue 3. general info 1. 1. apex - narrow superior region 2. 2. base - concave, inferior region 3. 3. root - area of attachment that includes bronchi, large blood vessels, and nerves 4. pleura - serous membranes that surround each lung 1. 1. two layers around each lung 2. 2. pleural cavity - space between layers, contains lubricating fluid Mechanics of Breathing 1. Inspiration 1. 1. pressure - collision of molecules within a space, at sea level the pressure is 760 mm of Hg, dependent on volume and temperature 2. 2. pressure gradient - a difference in pressures which causes molecules to move to restore a "normal pressure" 3. 3. a volume change in the thoracic cavity causes a pressure gradient and the movent of air into the cavity 4. 4. inspiration is an active process requiring muscle contraction 1. 1. diaphragm and est. intercostal muscles contract 2. 2. thoracic cavity expands (8 volume) 3. 3. pleural cavity pressure decreases 4. 4. lung surface is pulled outward, lung volume 8 5. 5. alveolar pressure decreases below atmospheric 6. 6. air rushes in 2. 2. 1. 2. 3. 3. 3. 1. 2. 3. 4. 5. 6. 7. 4. 4. 1. 2. 3. Expiration 1. expiration is a passive process, no muscle contraction required 1. 1. diaphragm and ext. intercostals relax 2. 2. thoracic cavity decreases in size 3. 3. pleural pressure increases 4. 4. alveolar press. greater than atmospheric 5. 5. air flows out 2. surfacants and lower pressure in pleural cavity prevent alveoli from completely collapsing 1. 1. atelectasis - collapsed lung 3. forced expiration - requires internal costals to contract Respiratory Volumes 1. spirometer - tool used to measure respiratory volumes 2. tidal volume (TV) - amount of air exchanged in normal breathing Î500 ml 3. inspiratory reserve volume (IRV) - amount of air that can inhaled forcibly over tidal volume Î3100 ml 4. expiratory reserve volume (ERV) - amt. of air that can be forcibly exhaled after a tidal expiration Î1200 ml 5. residual volume (RV) - air remaining in lungs after a forced expiration Î1200 ml 6. vital capacity (VC) - total amt. of exchangeable air (TV + IRV +ERV) 7. total lung capacity - VC + RV = air contained in fully inflated lung Î6000 ml Exchange of Gases 1. Partial Pressure 1. 1. air is a mixture of gases, the amount of pressure each gas exerts is called the partial pressure Px 1. 1. for O2 PO2 = 760mm Hg x 21% = 160 mm Hg 2. 2. gases diffuse along pressure gradient independently 3. 3. gases exist in various states within the bloodstream - dissolved in plasma, bound to proteins, combined w/ other chemicals 1. 1. only gases dissolved in plasma affect partial pressure 2. External Respiration 1. 1. exchange of gas between alveoli and blood across respiratory membrane 2. 2. relies on greater PO2 in alveoli than in blood plasma 3. 3. 98% of O2 in blood is bound to hemoglobin and doesn't affect PO2 4. 4. also relies on greater PCO2 in blood plasma than in alveoli 3. Internal Respiration 1. 1. exchange of gases between capillaries and body cells 2. 2. relies on partial pressures of gases in capillaries, interstitial fluid, and cells 3. 4. 5. 3. oxygen 4. carbon dioxide - moves from cytoplasm to interstitial fluid to blood plasma 1. 1. 60 - 70 % of CO2 in blood is carried as bicarbonate ions HCO3 2. 2. converted after in enters blood by carbonic anhydrase to carbonic acid which breaks down to bicarbonate ion 3. 3. CO2 + H2O 6 H2CO2 6 HCO3- + H+ 4. 4. reverse reaction takes place as blood enters lung capillaries 5. 5. prevents acidosis by removing H ions from blood 5. gas levels are monitored by chemoreceptors in major arteries and in the brain, response is under nervous control