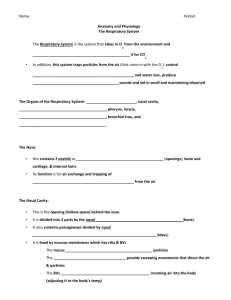
Lab Exer 9 Anatomy of the Respiratory System
advertisement

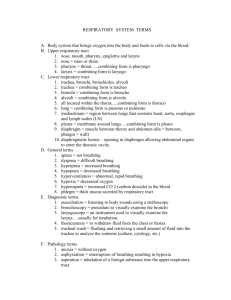
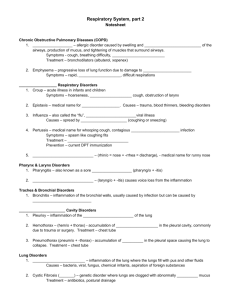
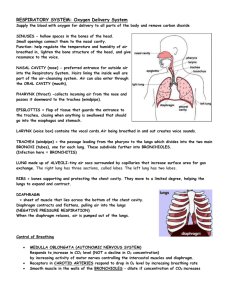
Laboratory Exercise 9: Anatomy of the Respiratory (Breathing) System The respiratory (breathing) system exchanges O2 and CO2 between the blood and the atmosphere. Cells obtain their energy from chemical reactions which require O2. Cells eliminate CO2, the gaseous end product of oxidative metabolism. Respiration can be explained in two ways: 1. the metabolic reactions of O2 with organic molecules, this is known as internal or cellular respiration. 2. the exchange of gases between the blood and the external environment, this is known as external respiration or breathing. A. Gross Anatomy of the Respiratory (Breathing) System The breathing anatomy is subdivided into a conducting division, which delivers or removes air, and a respiratory division, in which the gases are exchanged. Conducting Division – walls of tubes too thick for gases to diffuse across. During breathing, air enters the nose and mouth and is passed through a series of conducting structures until the air enters the air sacs. Nasal Cavity and Pharynx – The hard palate separates the nose from the mouth. The nasal cavity is lined with mucosa which warms and moistens the incoming air. The air then passes through the nasopharynx (a part of the pharynx above the soft palate), then through the pharynx proper (oropharynx), and into the lower respiratory tract. The lateral walls of the nasal cavity contain three bony projections (superior, middle, inferior nasal conchae). The nasal conchae are covered with mucosa and provide added surface area for warming and moistening inhaled air. Two auditory (Eustachian) tube openings are in the walls of the nasopharynx. Larynx – or “voice box” begins the tubular system or airways connecting the lungs. The thyroid cartilage, the largest of the laryngeal cartilages, is on the anterior and lateral surfaces of the larynx. It forms a protective enclosure. The thyroid cartilage has on its anterior surface the laryngeal prominence or “Adam’s apple”. Air passes through the larynx via the glottis, the opening of the trachea. The glottis is bounded by two pairs of membranous folds. The upper pair, the ventricular folds, is the “false vocal cords”. The lower pair, the vocal folds, is the “true vocal cords”. The true vocal cords vibrate to produce sounds. The epiglottis a flap of elastic cartilage, attached to the superior border of the thyroid cartilage, covers the glottis during swallowing to prevent drawing in by suction (aspiration) of liquids and solids into the breathing system. At the inferior end of the larynx is the cricoid cartilage. Trachea – lies between the lungs in the space of the thoracic cavity known as the mediastinum. The trachea is a flexible, cylindrical tube supported by regular arranged C-shaped rings of cartilage. 1 Bronchial tubes –The trachea branches into two primary bronchi (bronchus, sing.), one extending to each lung. The right bronchus is shorter, wider and more vertical than the left. The primary bronchi divide into smaller secondary (lobar) bronchi, each supplying a lung lobe. The secondary bronchi give way to tertiary bronchi, which lead into the bronchioles. On the medial side of each lung is the root or hilum, the area where major blood vessels and air passageways connect with the lungs. The bronchial tubes have their walls kept open by plates of hyaline cartilage with a folded mucosa. Blood vessels can be distinguished from bronchi by the blood vessels’ thinner, smoother walls. Pulmonary veins (red) are always located inferior to pulmonary arteries (blue). Pleurae - Visceral pleura covers the lung surface, the parietal pleura covers the inner surface of the thorax. Serous fluid produced by the pleural membranes eliminates friction between the lungs and the thoracic walls during breathing. Respiratory Muscles – To move air into the lungs, the dimensions of the thoracic cavity must be increased by the contraction of muscles. The diaphragm, a dome-shaped partition between the thorax and abdomen, is the principal muscle of respiration. The diaphragm and the external intercostals (between the ribs) muscles on contraction expand the thoracic cavity dimensions, creating a drop in lung air pressure required for inhalation. The diaphragm increases the superior-inferior dimensions of the thoracic cavity, while the external intercostals muscles elevate the ribs to increase the anteriorposterior dimensions of the thoracic cavity. The diaphragm’s innervation is by cervical nerves C3-C5 in the form of the phrenic nerves. Lungs – have 5 lobes, the right lung has 3 lobes and the left lung has 2 lobes. B. Microscopic Anatomy of the Respiratory (Breathing) System Trachea – mucosal epithelium is pseudostratified ciliated columnar with goblet cells. In the wall of the trachea there are C-shaped hyaline cartilage rings to hold the lumen of trachea open. Lung - 1. Bronchi – The mucosa is pseudostratified ciliated columnar epithelium. In the larger bronchi the lumen is held open by C-shaped cartilage rings, in the smaller bronchi, the lumen is held open by irregular scattered plates. 2. Bronchioles – The mucosa is ciliated columnar epithelium (pseudostratified to simple) with a longitudinal folded mucous membrane. Smooth muscle in the wall of the bronchioles to hold the lumen open. To distinguish the bronchiole from the artery – The bronchiole has longitudinal folded mucous membrane. The arterial wall appears smooth and lumen of the artery has blood in it, while the bronchiole is empty. 2 Respiratory Division – wall is thin enough for gases to diffuse. Alveoli – are clusters of air sacs lateral and distal to the respiratory bronchioles. The alveoli are thinwalled (simple squamous epithelium) and are closely associated with the thin-walled pulmonary capillaries. This anatomical barrier is 4 layers thick between the air and blood spaces and is easily crossed by O2 and CO2. The alveolus and capillary constitute the respiratory membrane. Type II alveolar cells (septal cells) – secrete a fluid containing phospholipids and lipoprotein, called surfactant. The surfactant lowers surface tension of the alveolar fluid at the air-water junction. This surface tension in the lungs would cause collapse of the alveoli. The surfactant reduces the surface tension. Also the stretched elastic fibers in the alveolar wall hold the alveoli open. 3