Respiratory Overview
advertisement

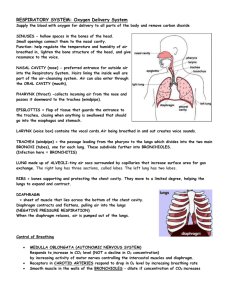
Respiratory Overview The respiratory system includes tubes that remove (filter) particles from incoming air and transport air into and out of the lungs. The system also includes many microscopic air sacs where gases are exchanged. The entire process of gas exchange between the atmosphere and body cells is called respiration. Events of respiration include: (1) movement of air into and out of the lungs-commonly called breathing or ventilation; (2) gas exchange between air and blood in the lungs; (3) gas transport in blood between the lungs and body cells; and (4) gas exchange between blood and body cells. Oxygen utilization and carbon dioxide production at the cellular level is called cellular respiration. The organs of the respiratory system include the nose, paranasal sinuses, pharynx, larynx, trachea, bronchi, and lungs. The parts of the respiratory system are frequently divided into the conducting division and the respiratory division. The conducting division of the respiratory system consists of those passages that serve only for airflow, from the nostrils through the bronchioles. The respiratory division consists of the alveoli and other distal gas exchange regions. The airway from the nose through the pharynx is often called the upper respiratory tract and the regions from the larynx through the lungs compose the lower respiratory tract. Air enters the respiratory system through the mouth or nose. These two pathways merge at the pharynx, which is also the path for food moving to the esophagus. The epiglottis lies at the top of the larynx, and by folding during swallowing, it prevents food from entering the respiratory passages. Air moves through the larynx into the trachea, which is stiffened by rings of cartilage. The trachea divides into two primary bronchi that enter the lungs. The bronchi are part of a highly branched system of air tubes referred to as the bronchial tree. The bronchial tree extends from the right and left primary bronchi to about 65,000 terminal bronchioles. Each terminal bronchiole branches into two or more smaller respiratory bronchioles, which mark the beginning of the respiratory division. The respiratory bronchioles divide into alveolar ducts which end in alveolar sacs. Alveoli are surrounded by capillaries and are the sites of gas exchange. Ciliated epithelium lines the primary bronchi through the terminal bronchioles. Cilia sweep foreign particles upward away from the lungs Respiratory Organs Bronchioles and Alveoli Alveoli, the sites of gas exchange between air and blood, are connected to respiratory bronchioles and alveolar ducts and are surrounded by capillaries. The alveolar epithelium consists primarily of simple squamous epithelium. Cells include: squamous (type I) alveolar cells: thin cells that allow for rapid gas exchange. great (type II) alveolar cells: cells that secrete surfactant, a chemical that reduces surface tension. alveolar macrophage: phagocytic cells. Alveoli are surrounded by capillaries. The mechanics of breathing involve changing the volume and pressure of the thoracic cavity. By using the principles of Boyle's Law, one can see that the pressure in the thoracic cavity is inversely proportional to its volume. When the intercostal muscles contract the ribs are elevated. At the same time the diaphragm contracts. These events expand the thoracic cavity, decreasing its internal pressure. The lungs expand, filling the thoracic cavity. The resulting pressure in the lungs is lower than that outside the body. Air enters the lungs until equilibrium is reached. When the diaphragm and the intercostal muscles relax, the thoracic cavity recoils. The resulting increase in pressure causes the air within the lungs to be expelled. The pressure of a given quantity of gas is inversely proportional to its volume. Increasing volume results in decreasing pressure. Decreasing volume results in increasing pressure. Increasing volume causes a decrease in pressure, which causes air to rush in as the pressures reach equilibrium. Decreasing volume causes an increase in pressure, which causes air to be expelled as pressures reach equilibrium. Air flows into and out of the lungs owing to a pressure gradient, between the atmospheric pressure and the intrapulmonary pressure. During inspiration, air flows from the atmosphere down a pressure gradient into the lungs, and during expiration, air flows from the lungs down the pressure gradient out to the atmosphere. This pressure gradient results from altering the volume of the thoracic cavity and thus altering the intrapulmonary pressure. Pressure Changes during Inspiration (a) Prior to inspiration, the intrapulmonary pressure is 760 millimeters of mercury (mm Hg). (b) The intrapulmonary pressure decreases to about 757 mm Hg as the thoracic cavity enlarges, and atmospheric pressure forces air into the airways. Muscles of Inspiration Quiet breathing occurs when the diaphragm and the external intercostals muscles contract. When the depth and frequency of inspiration increases, such as during exercise, the sternocleidomastoid and the scalenes muscles contract. Muscles of Expiration Normal quiet respiration results from relaxation of the diaphragm. Force expiration results when the internal intercostals and the abdominal muscles contract Breathing in, inspiration, is the result of a drop in pressure in the chest cavity and lungs. The decrease in intrapulmonary pressure is the result of increased volume due to movements of the diaphragm and ribs. The volume of the chest cavity increases, thus decreasing the intrapulmonary pressure. Air then flows from high pressure to low pressure. Breathing out, expiration, results when the diaphragm and ribs return to their relaxed positions and the volume of the chest cavity decreases. This increases the pressure inside the lungs and forces air out. Spirometry measures the amount of air inspired and expired. It can be used to diagnose respiratory disorders, such as asthma and emphysema. The following screens show spirograms for several breathing patterns. During normal breathing, approximately 500 milliliters of air are inspired and expired. This is called the tidal volume. During forced maximal inspiration, a quantity of air in addition to the resting tidal volume enters the lungs. This additional volume is called the inspiratory reserve volume, and equals about 3,000 milliliters. During a maximal expiration, about 1,100 milliliters of air in addition to the resting tidal volume can be expelled from the lungs. This quantity is called the expiratory reserve volume. However, even after the most forceful expiration, about 1,200 milliliters of air remain in the lungs. This is called the residual volume. During a combination of both forced inspiration and forced expiration, the inspiratory reserve volume is combined with the tidal volume and the expiratory reserve volume. This combination represents the greatest amount of air a person can inhale and exhale called the vital capacity. Lung Volumes and Capacities The tidal volume in the figure is the tidal volume during resting conditions. Respiratory capacities are obtained by adding two or more of the respiratory volumes. Control of Respiration Breathing is controlled by the medulla of the brainstem. It repeatedly triggers contraction of the diaphragm initiating inspiration. The rate of breathing changes with activity level in response to carbon dioxide levels, and to a lesser extent, oxygen levels, in the blood. Carbon dioxide lowers the pH of the blood. Regulation of Blood pH and Gases During gas exchange in the lungs, oxygen diffuses from the alveoli to capillaries while carbon dioxide moves in the opposite direction. The blood flow between the heart and the lungs is the pulmonary circulation. The tissues of the rest of the body are supplied by the systemic circulation. Oxygen diffuses to the tissues, and carbon dioxide diffuses from the tissues into the capillaries. The process of exchanging gases between the atmosphere and the body's cells is called respiration and involves several events, including breathing. As we zoom into the body we can observe the respiratory system during gas exchange. Air passes through the alveolar sacs to the alveoli, where gas exchange occurs. In this cutaway view of an alveolar sac and its capillary bed, the process of gas exchange is easily observed. During inspiration, atmosphere air fills the alveoli and gas exchange occurs between alveolar and capillary epithelia. Oxygen in inspired air is represented as a white gas. Carbon dioxide in expired air is represented as a blue gas. Notice the change in color in the red blood cells during gas exchange. Now let's zoom into a higher magnification view of gas exchange at the respiratory membrane. Red blood cells in the capillary adjacent to the alveolus release carbon dioxide and bind oxygen. Changes in the Partial Pressures of Oxygen and Carbon Dioxide 1. 2. 3. Oxygen diffuses into the blood and carbon dioxide diffuses into the alveoli because of differences in partial pressures. As a result of diffusion, the Po2 in the blood is equal to the Po2 in the alveoli, and the Pco2 in the blood is equal to the Pco2 in the alveoli. The Po2 of blood in the pulmonary veins is less than in the pulmonary capillaries because of mixing with shunted blood. 4. Oxygen diffuses into the tissue and carbon dioxide diffuses out of the tissue because of differences in partial pressures. As a result of diffusion, the Po2 in the blood is equal to the Po2 in the tissue, and the Pco2 in the blood is equal to the Pco2 in the tissue. Gas Exchange Each red blood cell contains 280 million hemoglobin molecules. Hemoglobin is folded protein with four iron-containing heme groups. Each heme unit binds with one oxygen unit. As a hemoglobin unit becomes oxygenated, its color changes to a brighter red. Collectively, this molecular color change is evident in the bright red color associated with arterial blood. Gas Transport Systemic Gas Exchange Cells are high in carbon dioxide and low in oxygen and each gas diffuses, following its concentration gradient. Note that CO2 loading releases hydrogen ions in the erythrocyte, and hydrogen ions promote O2 unloading Alveolar Gas Exchange In this lung capillary, oxygen is diffusing into the blood, and carbon dioxide is diffusing into the alveolus. .