The Lower Respiratory Tract Histology
advertisement

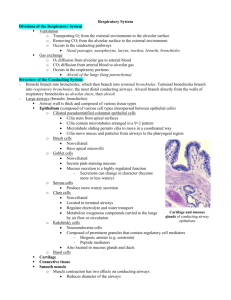
Histology Of The Lower Respiratory Tract First: Bronchioles -The bronchioles are divided into three parts: large, terminal, and respiratory. General characteristic of bronchioles: 1) The diameter: as we said before when we move distally in the respiratory tract the diameter decreases. -The diameter in the bronchioles is less than 5mm, because the last part in the bronchi has a diameter of 5mm. -The diameter of the large bronchioles is 1mm, 0.5mm for terminal bronchioles and less than 0.5 mm for respiratory bronchioles. 2) The bronchioles don't have glands, cartilage or lymphocytes. - Despite the fact that we have a numerous lymphocytes and lymphatic nodules in the distal part of the bronchus, in the bronchioles the lymphocytes were replaced by macrophages which were named, in the alveoli, dust cells. - There are only scattered goblet cells within the epithelium of the large bronchioles while the terminal and respiratory bronchioles are devoid from goblet cells. So saying that bronchioles in general don't contain goblet cells in their epithelium is a correct statement, but when we apply this statement to the large bronchioles only it will be incorrect, because it contains scattered goblet cell. 3) The epithelium: remember that we don't have abrupt changes in the respiratory tract. So from pseudostratified ciliated columnar to simple columnar ciliated then to simple cuboidal ciliated finally in the terminal part, esp. in the distal part of the terminal bronchioles and the respiratory bronchioles, the epithelium is formed mainly from Clara cells. - These Clara cells are simple cuboidal epithelium devoid from cilia and they contain secretory granules that contain substances which participate in the formation of the pulmonary surfactant which lines the apical surface of the alveolar epithelium to reduce the alveolar surface tension, so the formation of the surfactant is very important and must occur adequately before delivery to make the first inflation of the lungs passive (without any muscular effort from the baby). 4) The lamina propria: it contains a large amount of smooth muscle cells and elastic fibers. So in the case of Asthma there is a contraction of the smooth muscles in the bronchioles that can be relieved by the administration of sympathomimetic drugs like adrenaline causing bronchodilation. 5) The bronchioles also exhibit specialized cells called neuroepithelial cells, their number is between 80-100 cells, they receive cholinergic nerve endings, they contain secretory granules, and they also contain chemoreceptors. Second: The respiratory bronchioles - Around those bronchioles we will always find alveoli. The characteristics of the respiratory bronchioles: 1) The epithelium: is simple columnar or simple cuboidal and it may be ciliated or non-ciliated (Clara cells). 2) The smooth muscle cells: the amount of the smooth muscle cells will decrease gradually until they form knobs surrounding the openings of the alveoli that act as sphincters. Also we will have an increase in the elastic fibers and reticular fibers in the area between the alveoli to help in the inflation and deflation of the alveoli. The terminal part of the respiratory bronchioles is the alveolar ducts which will bifurcate distally to give the atria that communicate with the alveolar sac, so the end of the alveolar duct opens into the alveolar sac. Third: Alveoli - They are saclike evaginations; they have a diameter of 200μm. There are 300 million alveoli in each lung so the surface area is about 140m2. These alveoli are responsible for the spongy structure of the lungs because of the presence of elastic fibers and reticular fibers between the alveoli. -The space between two alveoli is called the inter-alveolar septum, within this space we have the interstitium which consist of capillaries and connective tissue, also within this septum there are alveolar pores which have a diameter between 10-15μm these pores equalize the alveolar air pressure and promote the collateral circulation between the alveoli esp. if there is a distal obstruction. 1) The wall of the alveoli contains: type 1 alveolar cells (type 1 pneumocytes) which are simple squamous cells and they form 97% of the wall, and type2 alveolar cells which form only 3% of the alveolar wall and they are present particularly at the corners of the alveolar wall .while in the interalveolar septum type 2 cells form16% of the septum (because of this they are also called septal cells) and type 1 form 8%. - Type 2 alveolar cells (septal cells) contain lamellar bodies which contain surfactant , the production of this substance will be increased in the last month before delivery, and as we mentioned this substance will line the inner aspect of the alveolar wall to form a surfactant film that reduces the surface tension . 2) The interalveolar septum: it's the septum between two alveolar walls starting from the epithelium of the first to the epithelium of the second (the epithelium of the alveolar walls are part of the septum) and within this septum we have the interstitium (capillary and connective tissue) also we have mast cells, fibroblasts (they form36%), elastic fibers, reticular fibers and macrophages (which form 10%). so the interstitium consists of : 1)capillaries 2)connective tissue which contains elastic fibers, reticular fibers, fibroblasts, and leukocytes. 3) The macrophages (dust cells): -They are derived from monocytes. - They are found in the interalveolar septum, in the alveolar wall and in the pleura. - in the case of congestive heart failure the lungs become congested with blood and some RBCs will enter the alveoli where they are phagocytosed by macrophages , as a result we will find those hemosiderin-laden macrophages (heart failure cells) in the sputum of the patients with heart failure . 4) The respiratory membrane (blood air barrier): consists of the epithelium of the alveolar wall and the endothelial cells of the capillary and between them there are fused basal laminae to decrease the thickness of the barrier and facilitate gas exchange, so the total thickness is around 0.1-1.5μm. This membrane permits only O2 to pass into blood capillaries and CO2 to diffuse in the opposite direction so this membrane is highly selective. The CO2 is released from the H2CO3 by the action of the carbonic anhydrase enzyme which is present within the erythrocytes. - The cells that form the respiratory membrane: - Type 1 cells (pneumocytes type 1): they form 97% of the alveolar wall, they are simple squamous cells, they are extremely attenuated cells, and their thickness is about 25nm. The organelles of those cells are grouped around the nucleus leaving a large portion of the cytoplasm free from organelles to facilitate gas exchange; also the cytoplasm contains abundant pinocytic vesicles which play a role in the turnover of the surfactant and the removal of small particulate contaminants. The lateral wall of those cells contains desmosomes and occluding junctions and these junctions are numerous between them and type 2 cells to prevent the leakage of tissue fluid into the alveolar air space. - Capillary endothelial cells: they are extremely thin, continuous, not fenestrated, and their organelles are clustered together to clear a space for gas exchange. - Type two cells (septal cells): they are interspersed among type 1 alveolar cells, with which they have occluding and desmosomal junctions. They are cuboidal cells resting on the basement membrane of the alveolar epithelium and they have the same origin as the type 1 cells that line the alveolar wall. They are found mainly at the angles of the alveolar wall. They divide by mitosis to replace their own population and the type1 population. In histological sections they exhibit a characteristic foamy or vesicular cytoplasm, and they have lamellar bodies which contain phospholipids, proteins and glycosaminoglycans, all those contents will form the pulmonary surfactant which lowers the alveolar surface tension, the deficiency of this substance in the newborn will cause “Respiratory Distress syndrome (RDS) of the newborn”. Those cells and type 1 cells are destroyed by the inhalation of NO2 gas. -The surfactant layer consists of an aqueous hypophase, lipid monolayer and several proteins. The functions of the surfactant are: - Decrease the surface tension of the alveolar cells, so less inspiratory force is needed to inflate the alveoli. - Stabilizing the alveoli; without the surfactant the alveoli would tend to collapse during expiration. - It also acts as bactericidal substance. - In fetal development, surfactant appears in the last weeks (last month) of gestation and the production of it is mainly by type 2 cells (which contain lamellar bodies). - The surfactant is not static but is constantly being turned over; the lipoproteins are gradually removed from the surface by the pinocytic vesicles of the squamous epithelium, by macrophages, and by type 2 alveolar cells. - During intrauterine life the fetus receives oxygen from his mother through the placenta, but after delivery the lungs must inflate and start working so the doctor will carry the baby from his legs and stimulate the respiratory center in the brain by patting his back, then the lungs will inflate and the baby will cry marking the beginning of respiration. This information is important because it can help in differentiate between stillborn babies and babies who have died after delivery; because if the baby wasn’t stillborn he would have breathed and his lungs would be inflated and their density would be lower (they contain air) so they would float if placed in water. After delivery the delicate body of the baby is covered with amniotic fluid and is therefore extremely slippery and handling the baby requires extra caution to avoid accidental injuries or deaths. - The synthesis of surfactant can be induced by the administration of glucocorticoids. Fourth: The pulmonary blood vessels -Within the lungs we have bronchopulmonary segments; each consists of alveoli and connective tissue that contains the segment's artery, vein, and lymphatic vessel. Within this connective tissue the pulmonary vein is in the lateral side while the bronchiole, the lymphatic vessel and the pulmonary artery are in the middle of the connective tissue (the branches of the artery are surrounded by the adventia of the bronchioles). - The circulation within the lungs includes both nutrient (systemic) and functional (pulmonary) vessels. The pulmonary arteries have thin walls as a result of the low pressure (25mm Hg during systole and 5mm Hg during diastole). Within the lung the pulmonary arteries accompany the bronchial tree, the arteries then give many branches that end into a network of capillaries that surround the alveoli. On the other end of this network the small venules will originate and those venules are found singly in the parenchyma then in the interlobular septum then after they leave the lobules they follow the bronchial tree toward the hilum and finally they end in the left atrium as the 4 pulmonary veins. Done by: Ibraheem Suleiman Obaidat