Chapter 19

Chapter 19
1.
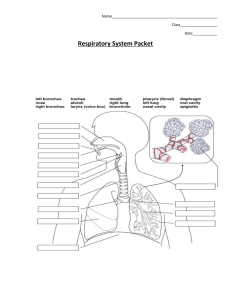
a. Pseudostratified epithelium—line the respiratory passageways; may have cilia that move mucus; the nuclei are located at two or more levels. b. Cuboidal epithelium—single layer of cube-shaped cells; carries on secretion and absorption. c. Simple squamous epithelium—single layer of thin, flattened cells; functions in gas exchange. d. Goblet cells—specialized, flask-shaped glandular cells; secrete a protective mucus. e. Cartilage—composed of fibers and gel-like ground substance; lack direct blood supply; provides a supportive framework. f. Smooth muscle—located in the walls of hollow internal organs; controlled by involuntary activity. g. Elastic fibers—a type of connective tissue; composed of microfibrils embedded in elastin; very elastic. h. Cilia—hair-like structures; move mucus upward and out of the airways. (Outcomes
3.2, 5.2, 5.3, 5.5, 19.3)
2.
Pursed lip breathing slows the flow rate of exhaled air. This creates a back pressure in the airways, which keeps the smaller airways open, preventing their collapse and obstruction. Thus, the lungs will “empty” more completely. (Outcomes 19.3, 19.4)
3.
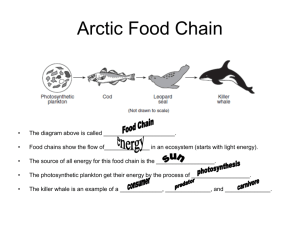
Concentration of blood oxygen would increase due to deep and rapid inhaling of air, which is 21% oxygen. Hyperventilation causes a decrease in blood carbon dioxide concentration. (Outcomes 19.3, 19.4, 19.5, 19.6, 19.7)
4.
Air entering a tracheostomy would not be warmed, filtered for removal of microorganisms and dust particles, or humidified by the nasal passages or oropharynx. The patient may experience irritation around and inside the tracheostomy opening (due to dryness), coughing, and respiratory infections. (Outcomes 19.3, 19.4,
19.6)
5.
Residual volume would increase due to overdistension of the lungs and loss of elastic recoil force from destruction of alveolar walls. This would increase pressure in the pleural cavity and inhibit expiration of air from the lungs. Expiratory reserve volume would be decreased due to loss of elastic recoil force of the alveoli. Vital capacity would decrease due to residual volume taking up more of the thoracic gas volume
(total lung capacity). Total lung capacity would remain the same or would increase due to overdistension of the lungs, increased anterior-posterior diameter of the chest wall, and increased residual volume. (Outcomes 19.3, 19.4, 19.6)
6.
The mixture of oxygen and carbon dioxide would be more beneficial. Carbon dioxide would normally stimulate the respiratory center and oxygen would prevent tissue hypoxia. (Outcomes 19.5, 19.6, 19.7)
7.
Respiration is controlled very closely by the chemoreceptors which sense the levels of carbon dioxide and oxygen in the blood. The main stimulus for respiration is an increase in carbon dioxide concentration in the blood. If you hold your breath, blood levels of carbon dioxide will increase. This will stimulate the chemoreceptors and the respiratory centers in the medulla to cause inspiration. Respiratory movements are
involuntarily controlled and thus you could not prevent inspiration. (Outcomes 19.5,
19.7)
8.
At high altitudes, the partial pressure of oxygen is less, which would stimulate chemoreceptors in the carotid and aortic bodies, resulting in an increased respiratory rate. If the individual is unable to breathe at this increased rate, oxygen will diffuse less rapidly from the alveoli into the blood and the tissues, including the brain, and the person will become hypoxic and lose consciousness. (Outcomes 19.6, 19.7)