Structure and Function of the Pulmonary System
advertisement

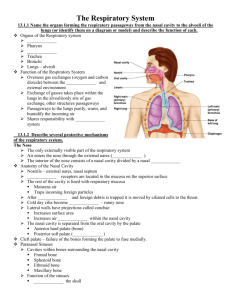
Structure and Function of the Pulmonary System Pulmonary System • Made up of two lungs – Where gas exchange takes place • Airways – To get air to lungs • Blood vessels – To circulate oxygen and carbon dioxide • Chest wall – To move air in and out of lungs through pressure changes and protect lungs Airways • Can divide respiratory system into two parts: – Upper respiratory tract : nasal cavity, pharynx – Lower respiratory tract: larynx, trachea, bronchi, bronchioles, alveoli • Upper respiratory tract serves to conduct air into the body, and filter, warm and humidify the air. Nasal cavity • Hairs and mucus serve to protect the respiratory system by trapping dust, organisms and foreign particles. Irritant receptors in nares remove substances by sneezing when irritated by chemical or mechanical irritants. • Mucous membranes of nasal cavity and paranasal sinuses warm and humidify the air. Turbinate bones increase surface area for this purpose. • Air then passes into the pharynx, which has three divisions: – Nasopharynx – pseudostratified ciliated columnar epithelium – Oropharynx - nonkeratinized stratified squamous epithelium – Laryngopharynx - nonkeratinized stratified squamous epithelium Larynx • Made up of 9 cartilages: – Epiglottis – Thyroid cartilage – Cricoid cartilage – Paired cartilages : cuneiform, arytenoid, and corniculate cartilages • Two sets of vocal folds: – Upper – false vocal cords – prevent passage of foreign substances into trachea during swallowing – Lower – true vocal cords – for formation of sounds vocalization Muscles of larynx • Internal laryngeal muscles control tension on vocal cords • External muscles move larynx as a whole during swallowing. Trachea • Held open by 20 “C” shaped cartilages. • Extends to about level of T5, add branches into two primary bronchi • Lined with pseudostratified ciliated columnar epithelium • Ridge called carina – mucous membrane here is most sensitive area for triggering cough reflex. Bronchi • Right primary bronchus is wider, shorter and more vertical • Enter lungs at hilus • Branch into secondary or lobar bronchi, then into • Tertiary or segmental bronchi • Bronchioles – no cartilage, smooth muscle, supply the alveoli Lungs • • • • Two lungs Right lung has 3 lobes and two fissures Left lung has 2 lobes and one fissure Blood vessels and bronchi enter at hilus Alveoli • Small, thin air sacs surrounded by a “hair net” of capillaries • Most of the walls of the alveoli are made up of simple squamous epithelium, called Type 1 alveolar cells. Gas exchange takes place through these cells Other cells of the alveoli • Type II alveolar cells produce surfactant (lipoprotein) to decrease the surface tension of water in the lungs – Premature infants – respiratory-distress syndrome of the newborn • Alveolar macrophages, or “dust cells” phagocytize foreign particles and microbes Respiratory membrane • Made of alveolar type I cell, endothelium of capillary and their basement membranes. • As thin as possible for gas exchange which takes place by diffusion from areas of high partial pressure to low partial pressure • Any disorder that thickens the membrane decreases gas exchange. • Usually, about one third of the pulmonary vessels are perfused at one time, so if right heart output increases does not increase arterial pressure in lungs, simply perfuse more vessels. • Lungs are surrounded by pleural membranes : parietal pleura and visceral pleura • Separate by the mediastinum • Enclosed in the thoracic cavity. Pulmonary ventilation (breathing) • Takes place by decreasing the pressure inside the thoracic cavity, and allowing atmospheric pressure to force air into lungs. • Thoracic cavity is expanded primarily by the contraction and lowering of the diaphragm, but is aided by expansion of chest by contraction of the external intercostal muscles. Expiration • Is normally a passive process due to the relaxing of the inspiratory muscles and the elastic recoil of the lungs. Respiratory volumes • Amount of air moved in and out of lungs • Tidal volume is the amount of air moved with a normal breath • Minute volume of respiration = tidal volume X breaths per minute Control of breathing • Both voluntary and involuntary • Respiratory center in the medulla oblongata controls breathing. • The dorsal respiratory group sets the basic rhythm of breathing. (ventral –strenuous ) • Receives input from peripheral chemoreceptors and from pneumotaxic area • Hering-Breuer reflex – stretch receptors in lung activate the pneumotaxic area, which inhibits insipiration – preventing over inflation of lungs. Central Chemoreceptors • Chemical influences: – Central chemoreceptors in medulla oblongata – Sensitive to changes in conc. of CO2 and pH – CO2 + H2O ↔ H2CO3 ↔ H+ + HCO3carbon + water carbonic hydrogen bicarbonate dioxide acid ion ion Peripheral Chemoreceptors • Carotid bodies and aortic bodies • Stimulated by oxygen concentration decrease • Send impulses to respiratory centers, and breathing increases • Not triggered until O2 is very low (50 mm Hg) Oxygen transport • Gases move down partial pressure gradient. • 98 % of oxygen is bound to the iron in hemoglobin as oxyhemoglobin (HbO2) • Rest is dissolved in plasma • 4 Iron atoms per hemoglobin molecule • 1 hemoglobin molecule can hold up to 4 molecules of oxygen • Amount of oxygen on hemoglobin is determined by partial pressure of oxygen. Carbon Dioxide Transport • 7 % is dissolved in plasma • 23 % combines with the amino groups of the hemoglobin forming carbaminohemoglobin • 70 % is converted to bicarbonate ions Control of pulmonary circulation • In most areas of the body, hypoxia causes vasodilation. • Low oxygen concentrations in the alveoli of the lungs cause vasoconstriction. • This sends blood to areas of the lung that have higher oxygen concentrations • Chronic alveolar hypoxia can lead to permanent pulmonary artery hypertension, which can lead to right heart failure. • Acidemia also causes pulmonary artery constriction