Epstein Barr Virus
advertisement
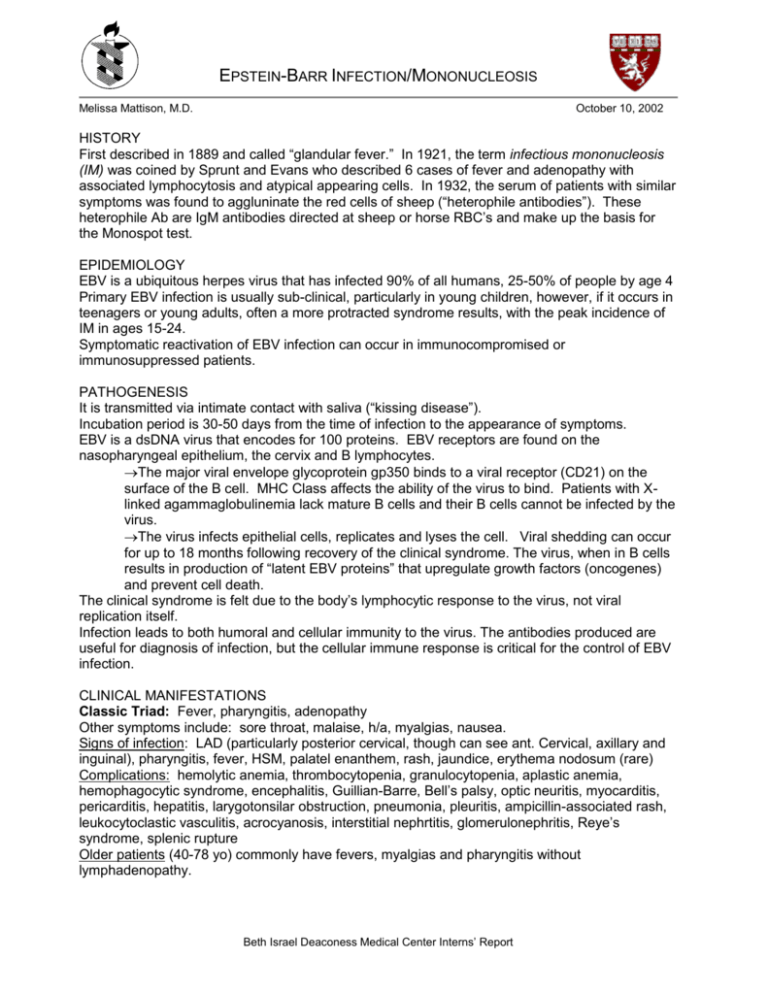
EPSTEIN-BARR INFECTION/MONONUCLEOSIS Melissa Mattison, M.D. October 10, 2002 HISTORY First described in 1889 and called “glandular fever.” In 1921, the term infectious mononucleosis (IM) was coined by Sprunt and Evans who described 6 cases of fever and adenopathy with associated lymphocytosis and atypical appearing cells. In 1932, the serum of patients with similar symptoms was found to aggluninate the red cells of sheep (“heterophile antibodies”). These heterophile Ab are IgM antibodies directed at sheep or horse RBC’s and make up the basis for the Monospot test. EPIDEMIOLOGY EBV is a ubiquitous herpes virus that has infected 90% of all humans, 25-50% of people by age 4 Primary EBV infection is usually sub-clinical, particularly in young children, however, if it occurs in teenagers or young adults, often a more protracted syndrome results, with the peak incidence of IM in ages 15-24. Symptomatic reactivation of EBV infection can occur in immunocompromised or immunosuppressed patients. PATHOGENESIS It is transmitted via intimate contact with saliva (“kissing disease”). Incubation period is 30-50 days from the time of infection to the appearance of symptoms. EBV is a dsDNA virus that encodes for 100 proteins. EBV receptors are found on the nasopharyngeal epithelium, the cervix and B lymphocytes. The major viral envelope glycoprotein gp350 binds to a viral receptor (CD21) on the surface of the B cell. MHC Class affects the ability of the virus to bind. Patients with Xlinked agammaglobulinemia lack mature B cells and their B cells cannot be infected by the virus. The virus infects epithelial cells, replicates and lyses the cell. Viral shedding can occur for up to 18 months following recovery of the clinical syndrome. The virus, when in B cells results in production of “latent EBV proteins” that upregulate growth factors (oncogenes) and prevent cell death. The clinical syndrome is felt due to the body’s lymphocytic response to the virus, not viral replication itself. Infection leads to both humoral and cellular immunity to the virus. The antibodies produced are useful for diagnosis of infection, but the cellular immune response is critical for the control of EBV infection. CLINICAL MANIFESTATIONS Classic Triad: Fever, pharyngitis, adenopathy Other symptoms include: sore throat, malaise, h/a, myalgias, nausea. Signs of infection: LAD (particularly posterior cervical, though can see ant. Cervical, axillary and inguinal), pharyngitis, fever, HSM, palatel enanthem, rash, jaundice, erythema nodosum (rare) Complications: hemolytic anemia, thrombocytopenia, granulocytopenia, aplastic anemia, hemophagocytic syndrome, encephalitis, Guillian-Barre, Bell’s palsy, optic neuritis, myocarditis, pericarditis, hepatitis, larygotonsilar obstruction, pneumonia, pleuritis, ampicillin-associated rash, leukocytoclastic vasculitis, acrocyanosis, interstitial nephrtitis, glomerulonephritis, Reye’s syndrome, splenic rupture Older patients (40-78 yo) commonly have fevers, myalgias and pharyngitis without lymphadenopathy. Beth Israel Deaconess Medical Center Interns’ Report Hemolytic anemia: 0.5-3% of all patients with acute EBV. Most are cold-agglutinins. Hemolysis develops during the second to third week of the illness and can last 1-2 months. Splenic Rupture: occurs b/c lymphocytic infiltration of the spleen weakens its structural integrity and the organ is growing rapidly. Fortunately, this complication is rare. Contact sports are to be avoided. Note, spontaneous rupture is as common as traumatic rupture in the setting of acute EBV infection. DIAGOSIS WBC – increased number of peripheral mononuclear cells and atypical lymphocytes. The atypical lymphocytes are mainly T-cells responding to EBV-infected B cells. Heterophile Antibodies, also called Paul-Bunnell antibodies, detected by the Monospot test: present in 90% of patients at some point in their illness. Can be negative initially and turn positive. Stays positive for 9 mo to 1 year. 95% sensitive, 93% specific. Delayed appearance can be associated with longer convalescence. EBV-specific Antibodies EB-VCA-IgM (viral capsid antigen) – highly sensitive and specific for acute IM, persist for 4-8 weeks. EB-VCA-IgG – persist for life and used as an epidemiolgic tool. EB-NA –EBV nuclear antigen – appears 3 wks after infection, peaks at 8 weeks and stays positive for life. EB-NA-IgG seen 6-12 wks after the onset of symptoms, positive results early in course of infectious illness rules out acute EBV as the cause. Stays positive for life. DIFFERENTIAL DIAGNOSIS In sero-negative syndrome, consider acute CMV, HIV, hepatitis and toxoplasmosis infection. TREATMENT Largely supportive and non-specific (fluids, analgesics, NSAIDs). Various antivirals (acyclovir, gancyclovir, alpha-interferon) have all been tried but none has shown clinical benefit Corticosteroids are indicated when impending airway compromise is possible, there is severe thrombocytopenia or hemolytic anemia. CANCERS ASSOCIATED WITH EBV Nasopharyngeal carcinoma – particularly in southern China, northern Africa and the Alaskan Eskimo population. Approx 100% of poorly differentiated nasopharyngeal carcinoma contain the EBV genomes and express EBV proteins. Burkitt’s Lymphoma: high-grade malignant lymphoma of small, non-cleaved B cells. In equatorial Africa, it’s associated with Plasmodium falciparum malaria. The malarial infection is thought to inhibit the T-cells ability to control the proliferating EBV infected B cells. Contain a chromosomal translocation resulting in up-regulation of the c-myc gene and increased tumorigenicity of the cells. Hodgkin’s Disease: EBV DNA is found in 40-60% of tumor in patient’s with HD in the USA. Lymphoproliferative Disease: associated with EBV in patients with immunodeficiency. EBV AND HIV Patients with AIDS have 10-20x more circulating infected B cells than healthy persons. They are prone to developing: Oral Hairy Leukoplakia Lymphoid Instersitial Pneumonia (particularly children with AIDS) Non-Hodgkin’s Lymphoma Virtually all primary CNS lymphoma in patients with HIV contain EBV DNA Beth Israel Deaconess Medical Center Interns’ Report