Infectios Mononucleosis & EBV Infection
Infectious Mononucleosis
& EBV Infection
Dave Rupar MD
3 April 2012
EBV- a herpesvirus
Large, ds DNA
Identified in 1964 from Burkitt’s lymphoma tissue
EBV- a herpesvirus
Ubiquitous
Problems for normal and immunocompromised hosts
Latent infection
Transformation of lymphocytes
Oncogenic potential
Spread of EBV
Spread by oral secretions
4-7 week incubation
Only 6% have identifiable contact
Viral shedding by:
50-100% IM
25% asymptomatic seropositives
50% renal x-plant
Epidemiology of EBV
50% seroconversion by age 5
College students seroconvert 12%/year
By age 25, 95% population is seropositive
A case, courtesy of HWC, MD
“I am the man”
A 16 year old boy, star of the football team, comes to see you because of sore throat for 5 days with mild fatigue,
I am the man...
PE:
Fever 102
2+ AC nodes, no rash or jaundice
Red throat with marked tonsillar exudate abdomen benign
I am the man...
LAB:
Rapid strep test negative
Monospot positive
Infectious Mononucleosis
Fever
Pharyngitis
Lymphadenopathy
Sumaya and Ench, Pediatrics 1985;75:1003
IM: other manifestations
Splenomegaly
Hepatitis
Rash
Anemia
Thrombocytopenia
Encephalitis
IM: other manifestations
Splenomegaly
Hepatitis
Rash
Anemia
Thrombocytopenia
Myocarditis
Encephalitis
By PE: 17%
By U/S: >95%
Average increase in size: 50%
Rupture is rare but exciting
IM: other manifestations
Splenomegaly
Hepatitis
Rash
Anemia
Thrombocytopenia
Encephalitis
Hepatomegaly 10%
Increased transaminases: 80%
Rarely severe
EBV not a cause of classic hepatitis
IM: other manifestations
Splenomegaly
Hepatitis
Rash
Anemia
Thrombocytopenia
Encephalitis
Ampicillin
Other antibiotics
IM: other manifestations
Splenomegaly
Hepatitis
Rash
Anemia
Thrombocytopenia
Encephalitis
AIHA 0.5-3%
Anti-i cold agglutinin
Hemophagocytosis
IM: other manifestations
Splenomegaly
Hepatitis
Rash
Anemia
Thrombocytopenia
Encephalitis
1-2 % of encephalitis
Clinical picture not well established
Clinical
IM: Diagnosis
DDx
GAS
CMV “mono”
Acute HIV syndrome
Adenovirus
Toxoplasmosis
Kawasaki disease
Malignancy
IM: Lab Diagnosis
Non-specific
CBC
LFT’s
Activated Cytotoxic T-lymphocytes =
“ Atypical Lymphs”
IM: Lab Diagnosis
Lab Diagnosis: Heterophile Ab
Paul & Bunnell, 1932: Serum from IM patients reacts with sheep blood
Monospot uses horse rbc’s
IgM polyclonal Ab
Does not react with EBV antigens
PPV 95% for EBV in patients with consistent illness
Lab Diagnosis: Heterophile Ab
False negatives
Too early (daysweeks)
Too young (<4 yo)
Heterophile neg mono: CMV, HIV, hep
B, toxo.
False positives
HPV B19, CMV, other viruses
SLE
Sarcoid
Lymphoma
Heterophile tests vary with age
EBV-specific Serology
EBV-specific Serology
Positive VCA IgM
Positive VCA IgG, negative EBNA = ?
Positive VCA IgG
Positive EBNA, negative VCA IgM =?
All negative =?
What can you learn from
EBV serology?
Recent infection - positive VCA IgM &
IgG, negative EBNA, variable EA
Old infection - positive VCA IgG and
EBNA, negative VCA IgM
Never infected - all negative
Do Not overinterpret- much variation in patterns
Beware of “chronic infection” or
“reactivation”
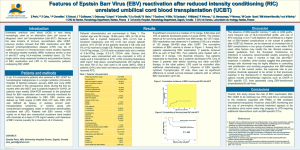
Detection of Virus: PCR
Primarily a research tool
Clinical application in PTLD, severely immunosuppressed patients
No standardization for use in mono syndromes
The natural history of mono
80
70
60
50
40
30
20
10
0
Dx 1 month 2 months 6 months
Rea et al. JABFP 2001;14:234
150 patients with IM, mean age 21+7
Fatigue
Adenopathy
ST
Labs quickly return to normal
70
60
50
40
30
20
10
0
Dx 1 mo 2 mo
Rea et al. JABFP 2001;14:234
150 patients with IM, mean age 21+7
6 mo
ALT inc
AST inc
AtyL, %
Back to the case:
You know that the most common serious complications are…
1. Airway obstruction
2. Splenic rupture
3. Liver failure
4. Lymphoproliferative disease
5. 1 and 2
I am the man...
6 days after first visit (11days into illness),
Dad (an MD) says son is well and wants to play football now
At recheck that day, he is well and has nl
PE
Should you let him play?
Complications after IM
Splenic rupture
Airway Obstruction
Fatigue
Complications after IM
Splenic rupture
Fatigue
Airway Obstruction
Spontaneous rupture
0.1%
40 years at Mayo
8116 IM
5 definite, 4 probable
LUQ pain
Consider non-op mgmt
Mayo Clin Proceed 1992;67:846
How soon can he safely return to sports after his mono?
1. 3 weeks
2. 4 weeks
3. 5 weeks
4. 6 weeks
5. 6 months
How to decide?
Clinical algorithm: Return to play
Auwater P. Infectious mononucleosis: Return to play. Clinics in Sports Medicine
2004; 23:485.
Thanks, Dr Henin
What about the Athlete? Part Deux
“Contact Sports should be avoided until the patient is recovered fully from IM and the spleen is no longer palpable.”
2009 Red Book , p 292
Complications after IM
Splenic rupture
Airway Obstruction
Fatigue
Acute Airway Obstruction
Little data
Rare (<1%?)
More common in young children?
Look for stridor, dyspnea
Monitor O2 sats
Steroids may be helpful in hospitalized patient
Complications after IM
Splenic rupture
Airway Obstruction
Fatigue
Complications after IM
Splenic rupture
Airway Obstruction
Fatigue
Generally “2-4 week” duration
1948: 25% persistent illness with fatigue at 3 mo.
2001:
2 mo- 38% not recovered
6 mo- 12% not recovered
Disease Profile in Male and Female Case Patients with
Infectious Mononucleosis
.
Macsween K F et al. Clin Infect Dis. 2010;50:699-706
© 2010 by the Infectious Diseases Society of America
“Chronic Mono”?
Fatigue after IM is common
Female sex, premorbid personality are risk factors
No evidence of ongoing viral replication or organ involvement
Prognosis is excellent
Encourage activity
Chronic Fatigue Syndrome
Fatigue is common in the adolescent/young adult population
More common after IM than other infections
Much is unexplained
“Abnormal” EBV AB no more common in CFS than in general population
“Necessary but insufficient”?
Don’t blame Lyme, either http://www.cdc.gov/cfs/
Contrast “Chronic Mono” with
Severe Chronic Active EBV Infection
X-linked Lymphoproliferative Syndrome
Virus-Associated Hemophagocytic
Syndrome
EBV: treatment
Supportive only in most cases
Acyclovir, etc. of limited value
Widespread belief in value of steroids despite suspicion of increased serious complications
Role for prednisone (1 mg/kg) in
UAO
Hemolytic anemia
Myocarditis
HPS
Does treatment work?
A: Duration of ST
C: Time away from school/work
94 patients, mean age 18, with IM.
Randomized, DB, PC Acyclovir + prednisone vs placebo. All results NS
Tynell et al. J Infect Dis 1996;174:324
EBV: treatment
“Although therapy with short-course corticosteroids may have a beneficial effect on acute symptoms, because of potential adverse effects , their use should be considered only for patients with impending airway obstruction, massive splenomegaly, myocarditis, hemolyic anemia or HLH.”
Emphasis added.
2009 Red Book, page 292
The End
?
Don’t forget to fill out your pathogen brackets!
SCAEBV
>6 months duration
Fever
Lymphadenopathy
HSM
Pancytopenia
Often fatal
High VCA IgG
High EA IgG
EBV DNA in tissue, blood
No HPS
Organ involvement
BM
Lungs
Hepatitis
Uveitis
Hemophagocytic Syndrome
Median age ~18 months
Primary (HLH) vs. secondary (VAHPS)
EBV one of identified causes
High fatality
FUO
HSM
Lymphadenopathy
Rash
Pneumonia
DIC
Clin Infect Dis 2003;36:306
Hemophagocytic Syndrome
Pancytopenia (>2 cell lines)
Elevated LFT’s, LDH
Coagulopathy
Hyperferritinemia
HP in BM, spleen, nodes
IM: Encephalitis
CEP: 17 patients with encephalitis due to
EBV
Median age 11 (1-31)
11 ICU
14 fever
11 seizure
4 coma
CSF
7 wbc ((0-2250)
Pro 37 (21-139)
Glucose normal
Young males
Severe, fatal IM
May have IAHPS
Hypogammaglobulinemia
NHL
XLP
Genetic Diagnosis
Family History
Graph showing correlation of initial fatigue score with the duration of fatigue (P=.023).
Macsween K F et al. Clin Infect Dis. 2010;50:699-706
© 2010 by the Infectious Diseases Society of America
EBV- associated malignancies
Burkitt’s lymphoma (African children)
NP carcinoma
CNS lymphoma in AIDS patients
Hodgkin’s lymphoma
EBV- a herpesvirus
Binds to CD21 receptor
(B-lymphocytes)
Up to 20% infected acutely
Most cleared
50/10 9 remain latently infected (episome)
Express only 10 genes
Lifelong reservoir