What Factors Contribute to the Risk for MS?

What Factors Contribute to the
Risk for MS?
Prevalence
Sex distribution
Age at onset
Ethnic origin
MS Epidemiology
~350,000 persons in the United
States
~75% female
Typically 20−40 years, but can present at any age
Predominantly Caucasian
Compston A, et al . McAlpine’s Multiple Sclerosis , 4 th ed. Churchill Livingston; 2006. Hauser
SL, et al. Multiple Sclerosis. In: Fauci AS, et al. Harrison’s Principles of Internal Medicine . Available at: http://www.accessmedicine.com/content.aspx?aID=2906448 . Accessed on: February 19, 2010.
Multiple Sclerosis
An Immunogenetic Disease
Environmental Factors
Genetic Predisposition
Immune Dysregulation
MS
Graphic courtesy of Suhayl Dhib-Jalbut, MD.
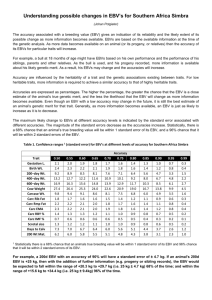
Evidence for Genetic Basis of MS
50
45
40
35
30
25
20
15
10
5
0
25%
5%
Identical
Twin
Fraternal
Twin
3%
2%
Sibling Parent or
Half-
Sibling
1%
First
Cousin
0.1% 0.1%
Spouse No
Family
Member
Hauser SL, et al. Multiple Sclerosis. In: Fauci AS, et al, eds. Harrison's Principles of Internal Medicine.
Available at: http://www.accessmedicine.com/content.aspx?aID=2906445. Accessed on: February 19,
2010. Willer CJ, et al. Proc Natl Acad Sci U S A.
2003;100:12877-12882.
Evidence for Environmental
Basis of MS
• No evidence of MS prior to 1822 (~ onset of industrial revolution in Europe)
• Change in the gender ratio over time
• These changes (eg, gender ratio, increasing incidence) took place over ~ 30 years (1 –2 generations) —too fast for a genetics cause
• Increased incidence of MS in many regions
(especially in women)
– When individuals migrate before age 15 from a region of high MS prevalence to one of low prevalence (or vice versa), they seem to adopt a prevalence similar to that of the region to which they moved
– When they make the same move after age 15, they seem to retain the risk of the region from which they moved
Multiple Sclerosis
What Are the Environmental Factors?
• Many environmental factors have been proposed
• Two currently popular candidates for involvement in MS pathogenesis are:
– Epstein-Barr virus (EBV) infection
– Vitamin D deficiency (sunlight exposure)
• These are hypotheses—not proven facts!
– Either, neither, or both may be correct
Evidence for EBV
• Indirect evidence
– Late EBV infection is associated with MS
– Symptomatic mononucleosis is associated with MS
• Direct evidence
– 10 out of 12 studies found a significantly higher rate of EBV positivity in MS patients than in controls 1-12
– When data from these 12 trials are combined
(N = 4155), EBV positivity is found in 99.5% of MS patients vs 94.2% of controls (P <10-23)
1. Sumaya, 1980. 2. Bray, 1983. 3. Larson, 1984. 4. Sumaya, 1985. 5. Shirodaria, 1987. 6.
Munch, 1998. 7. Myhr, 1998. 8. Wagner, 2000. 9. Ascherio, 2001. 10. Sundström, 2004. 11.
Haahr, 2004. 12. Ponsonby, 2005.
Worldwide Prevalence of MS
Latitude gradient for UVB is strikingly similar = indirect evidence for vitamin D hypothesis
≥30 per 100,000 population
5 –25 per 100,000 population
<5 per 100,000 population
Reprinted from Kurtzke JF. Acta Neurol Scandinav.
1980;62:65-80, with permission from Blackwell Synergy.
Direct Evidence for Vitamin D
• >185,000 women interviewed about their diet: Those in highest quintile of vitamin D consumption had significantly less new-onset MS compared with lowest quintile 1
• Study of MS patients and controls from Tasmania found significant negative association between total sun exposure during childhood (especially in those 6 –10 years old) and adolescence and the subsequent development of
MS 2,3
• Evaluation of stored serum samples from 257 MS patients and 514 matched controls (US Military) showed the risk of
MS was significantly decreased in those with increased serum vitamin D3 levels 4
1. Munger KL, et al. Neurology. 2004;62:60-65. 2. Van der Mei IA, et al. J Neurol. 2007;254:581-590. 3. Van der Mei IA, et al. BJM. 2003;327:316. 4. Munger KL, et al. JAMA . 2006;296:2832-2838.
Risk Factors for MS
Summary
• MS is caused by a complex interaction of genetic and environmental factors
– In someone with an affected identical twin, risk of
MS is 25%, suggesting that genetics play a role in susceptibility but are not the complete story
• Vitamin D insufficiency and EBV infection have shown possible links to MS
– This research is thought-provoking, but these factors have not been definitely proven as causes of MS
Pathophysiology of MS
Pathophysiology of MS
• Acute Inflammation
• Neuronal Degeneration
Relapses
Disability
Immune Dysregulation in MS
T Cells
• T cells normally recognize specific antigens
– CD8+ T cells destroy infected cells
– CD4+ T cells release cytokines that mediate inflammatory and anti-inflammatory responses
• T cells reactive to myelin are found in MS lesions, blood, and cerebrospinal fluid
– CD8+ T cells transect axons, induce oligodendrocyte death, promote vascular permeability 1
– There is a cytokine imbalance in MS, favoring secretion of inflammatory (Th1) cytokines
– T cells that normally regulate immune function have reduced activity in MS 2
1. Dhib-Jalbut S. Neurology. 2007;68:S13-S21. 2. Viglietta V, et al. J Exp Med. 2004;199:971-979.
Cytokine Imbalance in MS
Normal
T
H
1
T
H
2
Inflammatory Anti-inflammatory
IFNg
, IL-12, TNF IL-4, IL-10, TGFß
MS
T
H
2
T
H
1
Inflammatory
IFNg
, IL-12, TNF
Graphic courtesy of Suhayl Dhib-Jalbut, MD.
Anti-inflammatory
IL-4, IL-10,TGFß
Immune Dysregulation in MS
B Cells
• In some MS patients, ectopic lymphoid follicles have been found in the meninges 1
• Mechanisms of B cells in MS may include:
– Antimyelin antibody production
– Antigen presentation to autoreactive T cells
– Proinflammatory cytokine production
1. Uccelli A, et al. Trends Immunol . 2005;26:254-259.
Immune Dysregulation in MS
Other Involved Cells
• Natural killer (NK) cells
– May play opposing roles as both regulators and inducers of disease relative to cytokine environment and cell:cell contact
– NK cell function may be lost during clinical relapse
• Monocytes
– Secrete IL-6 (promotes B cell growth) and IL-2 (aids differentiation of Th1 cells)
• Macrophages
– Phagocytic activity may contribute to demyelination
• Microglia
– Specialized macrophages in the CNS, also may contribute to
T cell activation
Neurodegeneration
• Loss of axons is the main cause of permanent disability in MS
• Axonal damage has been shown to occur in acute inflammatory plaques 1 and can lead to brain atrophy
– Occurs in white and gray matter
– May also produce cognitive impairment
• Axonal damage could be the result of
– Cumulative inflammatory damage over time
– A parallel degenerative process related to loss of trophic support or an independent axonal degeneration 2
• Can effective immune therapy early in MS prevent worsening disability?
1. Trapp BD, et al. N Engl J Med.
1998;338:278-285. 2. Trapp BD. Neuroscientist.
1999;5:48-57.
Conclusions
• Pathogenesis of MS involves complex interactions between genetic and environmental factors
– Multiple genes are involved
– Vitamin D deficiency and EBV infection are 2 candidates
• MS incidence has increased over the past 30 years due to a change in environmental exposure
• MS pathogenesis involves multiple immune cell types
(T cells,
B cells, NK cells, others)
• Along with chronic inflammation, MS pathogenesis involves axonal loss
– Neurodegeneration is the major source of disability in MS