Upper GI Bleed
advertisement

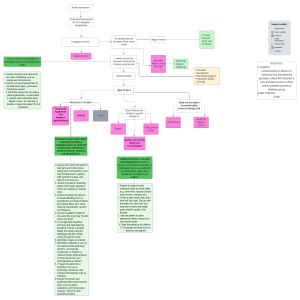
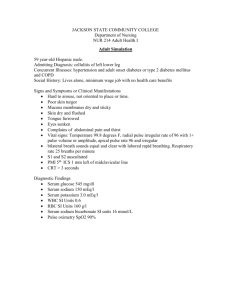
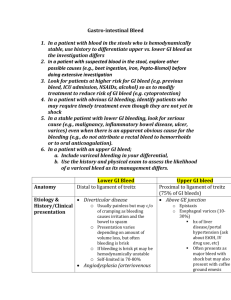
Upper GI Bleed Haematemesis – vomiting blood – bright red or coffee grounds Melaena – black motions often like tar – altered blood Both indicate upper GI bleed Causes: There are many causes for upper GI hemorrhage. Causes are usually anatomically divided into their location in the upper gastrointestinal tract. Patients are usually stratified into having either variceal or non-variceal sources of upper GI hemorrhage, as the two have different treatment algorithms and prognosis. Gastric ulcer in antrum of stomach with overlying clot. Pathology was consistent with gastric lymphoma. Reproduced with permission of patientThe causes for upper GI hemorrhage include the following: Esophageal causes: Esophageal varices Esophagitis Esophageal cancer Esophageal ulcers Gastric causes: Gastric ulcer Gastric cancer Gastritis Gastric varices Gastric antral vascular ectasia, or watermelon stomach Dieulafoy's lesions Duodenal causes: Duodenal ulcer Vascular malformations, including aorto-enteric fistulae. Fistulae are usually secondary to prior vascular surgery and usually occur at the proximal anastomosis at the third or fourth portion of the duodenum where it is retroperitoneal and near the aorta.[1][2][3] Hematobilia, or bleeding from the biliary tree Hemosuccus pancreaticus, or bleeding from the pancreatic duct History Previous GI bleeds, dyspepsia, known ulcers Known liver disease or varices Dysphagia, vomiting, weight loss Check drugs and alcohol consumption Any serious co-morbidity – worse prognosis Examination Signs of chronic liver disease PR to check for melaena Is the patient shocked? Faint when sits up, peripherally cool and clammy, prolonged capillary refill Assess GCS Poor urine output e.g.<25ml/h Tachycardia (with JVP not raised) Hypotensive or postural drop in BP Calculate Rockall Risk Score 0 pts Pre-endoscopy Age <60 Systolic BP Sys BP <100 (shock) and PR <100 pulse Co-morbidity Nil major Post-endoscopy Diagnosis Recent haemorrhage on endoscopy Mallory-weiss No lesion No recent bleed None or dark red spot 1 pt 2 pts 60-79 BP>100 PR>100 >80 BP<100 Cardiac failure IHD Renal failure Liver failure All other diagnoses Upper GI malignancy 3 pts Metastases Blood in upper GIT, adherent clot, visible vessel Acute Management Protect airway and give high flow oxygen 2 large bore IV cannulae and take blood for FBC (early blood may be normal), U+E (high urea out of proportion to creatinine is indicative of a massive blood meal), LFT, clotting and cross match 4-6 units Give IV crystalloid to restore intravascular volume while waiting for blood to be cross-matched: in dire emergency give group 0 rh –ve Insert a urinary catheter and monitor hourly urine output Organise CXR, ECG, check ABG Consider CVP line to monitor and guide fluid replacement Transfuse with cross-matched blood until haemodynamically stable Monitor pulse, BP, CVP at least hourly Urgent endoscopy Inform surgeons Further Management Re-examine after 4 hours and give FFP if >4 units transfused Monitor observations and urine output hourly, if stable – 4 hourly Keep haemoglobin >10g/dl – keep 2 units in reserve Give omeprazole 40mg IV after endoscopy (reduces risk of re-bleed and need for surgery) Check FBC, U+E, Clotting Nil by mouth for 24 hrs, clear fluid after 24 hours, light diet after 48 hours as long as no evidence of re-bleed Endoscopy Arrange after resuscitation, within 4 hrs of suspected variceal haemorrhage, or when bleeding ongoing within 24 hours admission It can identify site of bleed, estimate risk or re-bleed, administer treatment, preferably 2 of adrenaline, sclerotherapy, variceal banding or argon plasma coagulation Endoscopic signs Active arterial bleed, visible vessel, adherent clot/black dots Re-bleed 40% die of complications Identify high risk patients and monitor closely for signs of re-bleed IV omeprazole has a preventative role Get help – inform surgeon at once if Haematemasis and melaena Tachycardia Reduced CVP Reduced BP Reduced urine output Indications for surgery Onset of severe re-bleed despite 6U transfusion if >60 yrs Re-bleeding Active or uncontrollable bleed at endoscopy Initial Rockall score>3 or final score>6 Varices Portal hypertension causes dilated collateral veins at sites of portosystemic anastomosis Most commonly form in lower oesophagus but can also be found around umbilicus (caput medusae) and in the rectum Develop in patients with cirrhosis once portal pressure is >10mmHg If >12mmHg, bleeding may develop- associated with mortality of 30-50 % per episode Other causes of portal hypertension Pre-hepatic – portal vein thrombosis, splenic vein thrombosis Hepatic – cirrhosis, shistosomiasis, sarcoidosis, myeloproliferative disorders Post-hepatic – Budd-Chiari syndrome, Right heart failure, constrictive pericarditis, veno-occlusive disorders Suspect varices if alcohol abuse or cirrhosis – look for signs of chronic liver disease, splenomegaly, encephalopathy, ascities, coagulopathy and thrombocytopenia Prophylaxis Primary – non-selective beta blockade – propranolol 40-80mg/12h po Repeat endoscopic banding ligation Secondary – same as above plus transjugular portosystemic shunt if resistant to banding Acute management of variceal bleed Resuscitate until stable (do not give saline) Correct clotting abnormalities with vitamin K and FFP IV terlipressin 2mg bolus Endoscopic banding or sclerotherapy If bleeding uncontrolled – sengstaken-blakemore tube – balloon tamponade