UPPER GI BLEED
advertisement
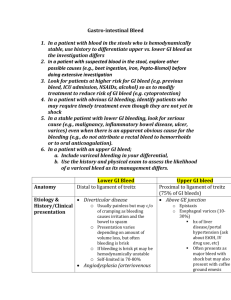
UPPER GI BLEED Kate Edwards FY1 Doctor DEFINITION Any bleed from the GI tract proximal to ascending part of the duodenum (final ¼). A major cause of emergency admissions to hospitals. 5-10% mortality depending of level of bleeding and cause. CAUSES Mallory-Weiss Syndrome 2% Gastric Ca 2% Other 10% Oesophagitis 11% Oesophageal Varicies 45% Gastric Erosion 13% PUD 17% OTHER Includes iatrogenic induced such as NSAID or poorly controlled anticoagulant use. Rarely this also includes a Cushing ulcer due to over use of steroids. Also cases were causes are not found. HX OF BLEEDING Haematemisis: - fresh red blood in vomit or coffee ground. - Indicates bleeding from the oesophagus or stomach. -May be recurrent minor episodes; however one major episode my compromise airway. Malaena: - Offensive black tarry stools. - Indicates bleeding from after the pyloric sphincter. - May also indicate Lower GI bleed. - Ensure patient is not on iron tablets. ASSOCIATED SYMPTOMS Anaemia if chronic bleeding Collapse/shock if major bleed Weakness/dizziness Palpitations Sweating Weakness Hx of dypepsia Hx of epigastric pain Hx of NSAID use Hx of alcohol abuse EXAMINATION ONLY if patient is haemodynamically stable, otherwise treat first then examine for cause when stable. Hands – look for liver signs such as liver flap, and palma erythema. Pulse and BP - to asses patients haemodynamic status, early warning is rise in HR, later is drop in BP. Face – for anaemia and jaundice in sclera. Chest/arms – spider neva. Abdo – Ascities, caput medusae, epigastric tenderness, feel for aortic aneurysm/hepatomegaly. PR – feel for haemorrhoids, stool in INITIAL MANAGEMENT IN MAJOR BLEED ASSESS ABC. Airway – Ensure airway is secure, use suction to remove blood/vomit, if compromised insert airway adjunct. Breathing – High flow oxygen 15lt at 100%, check sats. C – Insert two large bore cannulas, restore circulating volume using colloids/O negative blood, then cross matched 4-8 units (takes approx 45-60 mins). Bloods – FBC, U&E, Glucose, LFTS, Coag screen, G&S. Catherterise – monitor urine output (aim for >30ml/hr) NG tube after resus to assess severity. If clotting deranged the use vit K/FFP. ESTABLISH DIAGNOSIS Via OGD endoscopy. Only to be done once patient is haemodynamically stable. To be under taken within 24hrs of admission, in severe upper GI bleed should be within 4 hrs. Advantages of endoscopy: - Assess severity of bleeding. - Identify cause of bleeding. - Identify whether patient is suitable for surgery. - Perform basic management of cause. - Test for H.pylori. ENDOSCOPIC DIAGNOSIS PUD Oesophageal Varices Mallory-Weiss Tear OESOPHAGEAL VARICES Over distended veins caused by the formation of shunts due to portal hypertension. Shunt varicies are common in the oesophagus, superfical veins (caput medusae) and rectum (hemarroids). Portal hypertension is caused by chronic liver disease/cirrohsis (usually due to alcohol abuse) Enlargement of the liver causes increased pressure within the portal system leading to shunt formation. SPECIFIC MANAGEMENT OF VARICES Terlipressin given at presentation to reduce portal pressure. Prophylactic antibiotic therapy. Balloon tamponade should be considered as a temporary salvage treatment for uncontrolled variceal haemorrhage. Endoscopy: Band Ligation Injection of N-butyl-2-cyanoacrylate If fail then Transjugular Intrahepatic Portosystemic Shunt (TIPS) formation. PEPTIC ULCER DISEASE A break in the continuity of the epithelium in the stomach or duodenum. Causes include: H. Pylori infection, long term NSAID/Steroid use, smoking/alcohol/stress and ZollingerEllison syndrome. Clinical Features include – dyspepsia, waterbrash, epigastric tenderness, related with eating. H. Pylori infection is the commonest cause as it is found in 90% of patients with PUD, can be tested for via breath test or biopsy during OGD. Complications include haemorrhage, perforation or pyloric stenosis. SPECIFIC MANAGEMENT OF PUD Reduce risk factors. Initially Antacids, PPI, H2 receptor antagonist. Eradication of H. Pylori via triple therapy for 1 week: PPI e.g. Omeprazole/lansoprozle Amoxicillin Clarithromycin Endoscopy: Injection of adrenaline around ulcer Electrocoagulation Laser Coagulopathy Surgery may be required to over sew ulcer. MALLORY-WEISS TEAR Occurs at Gastro-oesophageal junction. Caused by excessive and prolonged vomiting/retching often following large bouts of alcohol consumption. Vomit is initially normal then bright red. Most stop spontaneously however endoscopic clipping or surgery may be required. RISK OF RE-BLEED: ROCKALL SCORE Score of <3 is minor, >8 is major. Mortality if approx: 3 pts – 10%, 5pts – 40%, 7 pts – 50% MILD TO MODERATE Admit to general medical ward. Observe for continued bleeding or re-bleeding. Endoscopy within 24 hrs and repeat in 6 weeks. Discharge when stable/no evidence of rebleed. SEVERE Admit to HDU. Observe closely for continuation of bleed/rebleed: HR/BP UO CVP Restore blood volume with IV fluids. Keep patient fasted. Emergency endoscopy. CASE 1 65 yr old man admitted with coffee ground vomit. C/O mild weakness/feeling faint for 3/7 Also notices possible dark colour to stools. H/O dypepsia. Smoker and drug hx takes NSAIDs for joint pain. O/E MEWS 0, tender epigastric region, pale sclera. Initial Diagnosis? Investigations? Management? CASE 1 Likely diagnosis PUD. Must assess ABC and ensure patient is stable. Investigations: Erect CXR and AXR to exclude perforation. Bloods – FBC, U&Es, LFTs, coag screen, G&S. Management: IV PPI and omit NSAIDs Endoscopy within 24hrs including possible treatment. If H. Pylori positive then triple therapy. CASE 2 48 yr old man admitted with sever haematemesis. Patient is tachy with drop in BP. Pt has yellow sclera and spider neva on torso. PMHx of liver failure, sever alcohol abuse. Likely Diagnosis? Immediate management? CASE 2 Likely to be varices bleed. Initial management is to assess via ABC. Ensure airway maintained. Give O2 and monitor sats. IV access with colloid/o negative blood until cross match (4-6units) Give terilpressin and emergency endoscopy. If airway compromised then balloon tamponade. Insert Catheter and NG. Admit to HDU. Endoscopy finds: Varices and major haemorrhage in gi tract. Rockall Score? CASE 2 CASE 2 Rockall Score: Age: 48 - 0 Shock: Hypotensive - 2 Co-morbidity: Liver failure – 3 Diagnosis: Varices – 2 Major SRH: Blood in Gi tract – 2 Total = 9/11 Severe bleed, mortality rate of 50% and high risk of re-bleed. Needs HDU input and close monitoring. ANY QUESTIONS?