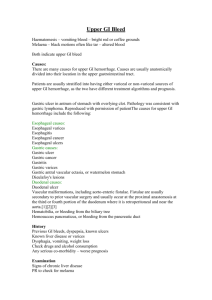
Portal Hypertension Portal blood flow backed up into esopagheal anastomoses Diagram Key (Beta) Disease Process Signs & Symptoms As variceal pressure increases blood vessel swells Esopagheal Varices - CT Scan, - Physical Exam, and - Hx Taking Bigger Varices Nursing Dx Nursing Responsibilities Diagnostic Tests Complication Medication Dilation of veins Increase vessel size Decrease wall thickness Increase vessel tension Risk for Bleeding r/t secondary to esophageal varices aeb swollen lymph nodes 1. Assess vital signs and observe for any signs of bleeding such as melena and hematemesis. 2. Perform a focused assessment on the abdominal region, particularly checking for ascites. 3. Administer drugs that can reduce portal hypertension, as prescribed. 4. Explain what endoscopic band ligation means, its risks and its benefits. Prepare the patient for the procedure. Red wave Markor Cherry Red Spot - Endoscopy - Capsule Endoscopy PROGNOSIS: - Variceal Rupture Octreotide Vassopressin Beta Blocking Agents: Propanolol, nadolol, carvedilol Upper GI bleed Blood loss in circulation Tachycardia hypotension SOB Weakness Lightheadedness Anemia Blood oxidized and vomitted or passed trhough GI Death Hematemesis Melena Decreased Cardiac Output related to bleeding secondary to esophageal varices as evidenced by tachycardia, hematemesis, shortness of breath, weakness and ligtheadedness. 1. Assess and monitor the patient?s vital signs and mental status. Taking note of the patient?s heart rate, blood pressure, capillary refill, peripheral pulses, and state of consciousness. 2. Assess the patient?s breathing pattern and oxygen saturation. Check for coughing or choking signs. 3. Assess the patient for signs of increased bleeding such as hematemesis (vomiting of blood) and melena (black tarry stool). Note the characteristic, amount, and frequency. 4. Assess the patient?s weight at the same time every day. Record intake and output 5. Encourage deep breathing exercises and diaphragmatic breathing. Instruct to breathe deeply and slowly using the diaphragm and then exhale slowly through the mouth. 6. Administer oxygen as ordered. 7. Administer medications such as non-selective beta-adrenergic blockers, somatostatin, vasopressin, or nitrates as ordered.Prepare blood products for blood transfusion and anticoagulants as ordered. 8. Prepare the patient for a procedure such as an endoscopy, ultrasound, and computed tomography scan as indicated. 9. Educate the patient and significant others about warning signs such as cardiac, respiratory, and mental status changes. Instruct to seek treatment promptly. Blood loss too rapid to be oxidized before emesis or passage of gi Coffee ground emesis Nausea and vomiting Weight loss Loss of appetite Imbalanced Nutrition: Less than Body Requirements related to digestive tract bleeding secondary to esophageal varices, as evidenced by hematemesis, weight loss, nausea and vomiting, loss of appetite. 1. Explore the patient?s daily nutritional intake and food habits (e.g. meal times, duration of each meal session, snacking, etc.) 2. Create a daily weight chart and a food and fluid chart. Discuss with the patient the short term and long-term nutrition and weight goals related to peptic ulcer disease. 3. Help the patient to select appropriate dietary choices and limit alcohol intake. 4. Refer the patient to the dietitian. 5. Encourage soft foods such as bananas and yogurts. Bright red blood per rectum IF TREATED: variceal ligation is effective in controlling first-time bleeding episodes in about 90% of patients. Liver transplant severe cirrhosis and/or repeated episodes of bleeding varices IF NOT TREATED: Death