GI Bleed
advertisement

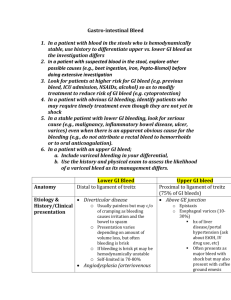
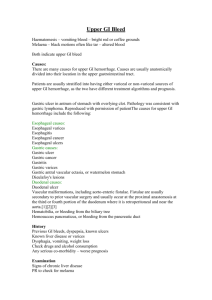
GI Bleeding: From Mouth to Rectum and Everywhere in Between Outline • • • • • • Epidemiology and Risk Factors Signs and Symptoms Physical Exam Findings Etiologies Diagnosis Management Will focus mostly on inpatients Epidemiology Key Point: Mortality LGIB < UGIB < Variceal bleeds • Upper GI bleeds (UGIB) ▫ 100,000 admissions/year to US hospitals ▫ 10% mortality • Variceal bleeds ▫ 30% of identified varices will bleed in 1 year ▫ 33% mortality with each bleed • Lower GI bleeds (LGIB) ▫ Less common than UGIB ▫ 3% mortality Key Point: Risk Factors Most Important Part of History! • • • • • • NSAID Use Cirrhosis Anticoagulation/Coagulopathy Age Risk factors for colon cancer Previous history of GI bleeding Signs and Symptoms Upper GI Bleed ▫ ▫ ▫ ▫ ▫ ▫ ▫ Lightheadedness/Syncope Diarrhea Anemia Hematemasis Melena Stigmata of cirrhosis Heartburn Lower GI Bleed ▫ ▫ ▫ ▫ Lightheadedness/Syncope Diarrhea Anemia Hematochezia Physical Exam Findings • • • • • • • • Vital signs (more later) Dry mucus membranes Stigmata of cirrhosis Fetid breath DRE – gotta do it Weak pulses Cool skin Encephalopathy Common Etiologies Upper GI Bleed Lower GI Bleed • • • • • • • • Diverticular disease – 30% • Colitis – 18% ▫ Ischemic ▫ Inflammatory ▫ Infectious • Neoplasms – 10% • AVMs – 8% • Hemorrhoids – 5% • Others – 20% PUD – 55 % Varices – 14 % AVMs – 6% Mallory Weiss Tears – 5% Tumors/Erosions – 4% Dieulafoy’s lesions – 1% Others 15% Khilani et all, Emerg Med 37(10):27-32, 2005 Diagnosis • Upper or Lower? ▫ History ▫ Digital Rectal Exam ▫ Hemoglobin • Still bleeding? ▫ Consider NG Lavage • What’s the etiology? ▫ Diagnostic Testing Freebees These can usually make the diagnosis Diagnostic Testing • • • • EGD – standard for UGIB Colonoscopy – standard for LGIB Push Enteroscopy – can image through SB Capsule Endoscopy – good yield - can’t intervene • Sigmoidoscopy – rarely used • Barium studies – good to look for lesions/mass • Tagged red cell scans – poor yield For more information, do a GI fellowship! Management – General Principles • Risk stratify ▫ Assess blood loss ▫ Blatchenford score Beyond the scope of this discussion! ▫ Rockall score (after EGD) • • • • IV access Volume replacement Acid suppression therapy Plan for diagnostic procedure Management: Assess Blood Loss Categor y % loss HR BP Pulse Pressure UOP Stage 1 <15 % < 100 Normal Normal > 30 Stage 2 15-30% > 100 Normal Decreased 20-30 Stage 3 30-40% > 120 Decrease d Decreased 5-15 Stage 4 > 40%Life >Support 140 Guidelines Decrease From Advanced Trauma Decreased Negligible d HR not useful if patients are on AV node blockers Tachycardic means they have lost about 1 liter of blood! Key Points If they are hypotensive, you are in trouble! Management: Access and Volume • IV Access ▫ Two large bore peripheral IVs is best • Volume replacement ▫ Normal saline ▫ Blood products ▫ Consider FFT/Cryo/FFP MGMT: Acid Suppression • Applies to UGIB from ulcers Key Point: PPIs can improve mortality Gralnek I.M et al. NEJM 2008 MGMT: Acid Suppression (con’t) • Other questions: Continuous versus bolus? IV versus oral? Duration of treatment? Management – Suspected Varices • Initial stabilization • Splanchnic Vasoconstricters: Octreotide/Vasopressin • TIPS • Minnesota tube/Blakemoore tube • Antibiotic prophylaxis • A whole other talk Key Points • GI bleeding is a common hospital diagnosis – Look for it • Risk factors are the most important part of the history • Vital signs can help risk stratify patients • PPIs can reduce need for surgery, rebleeding, and death