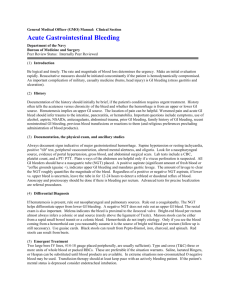
Acute Gastrointestinal Hemorrhage Outline
advertisement

Acute Gastrointestinal Hemorrhage Introduction o Medical emergency o Common complication of critical illness o Bleeding from upper or lower GI tract o Ligament of Treitz: (suspends the intestines and is attached to the diaphragm) Bleeding proximal to ligament: Upper GI Esophagus, Stomach, and Duodenum PUD, SRES, Varices, Mallory Weiss Tears Bleeding distal to ligament: Lower GI Jejunum, Ileum, Colon, and Rectum Diverticula, Cancer, Inflammatory disease o Gastric Parietal and Mucous Cells Parietal cells make hydrochloric acid Mucus creates the barrier that protects our stomachs Functions of Gastric Parietal Cells o Parietal Cells– forms HCl Acid Breaks down food and protein bonds o pH in the stomach is low (acidic), about 1.5 to 2 from the hydrochloric acid. Need proton pump to push new hydrochloric acid into the already acidic environment of the stomach. An H2 inhibitor slows production of hydrochloric acid, PPI prevents transport into the stomach Functions of Gastric Mucous Cells o Glycoprotein mucus - forms gel Maintains mucosal-luminal pH gradient o Epithelial mucous cells - secretes bicarbonate Augments action of glycoprotein mucus o Epithelial cell structure Protects against damage of gastric secretions Etiology of Upper GI Bleed o Peptic Ulcer Disease (PUD) Patho Breakdown of gastro-duodenal mucosa gastric secretions auto-digest layers of stomach damages blood vessels hemorrhage Primary Causes NSAIDS Helicobacter pylori o Bacteria from food, contaminated o Likes to get into the stomach and lives in the mucousal lining, acts as an agent that penetrates the epithelial layer, lets the acid come in and deteriorate the lining o Stress-Related Erosive Syndrome (SRES) Patho Stress ulcer Develop rapidly within hours Limited to the stomach Primary Causes: Increased acid production Decreased mucosal blood flow High Risk Patients: Post-op, Trauma, Shock, Burns (very susceptible), Acute Neurological Disease o Esophageal Varices Portal hypertension Vessels become engorged and dilated (varices) vulnerable to damage from gastric secretions rupture and hemorrhage Etiology of Lower GI Bleed o Diverticula Patho Sac-like herniation of the lining of the small intestine or colon - Sigmoid Colon most common High fat-Low fiber diet lead to weakening of lining Leads to inflammation, bleeding, perforation Caused by high fat / low fiber diet Complication of this is the diverticula perforating Assessment o o To Take away from this slide: HR. RR. urine output. Hypotensive. Confused. Lethargic. Skin: Cool & pale Assess Type of Bleeding Upper GI Bleed S/S Hematemesis (two kinds) o Bright red: Profuse bleeding ( acid contact) Varicies Coffee-ground: Slow bleed ( acid contact) o Gastric acid converts bright red hemoglobin to brown hematin PUD Melena o Digestion of blood from an upper GI bleed May take several days to clear after the bleeding has stopped Looks like tar Lower GI Bleed S/S Hematochezia o Massive lower GI hemorrhage Blood in GI tract increases peristalsis and diarrhea Red colored Blood streaked stool o Hemorrhoids – aka “Piles” Assess Lab Studies o o If the guaiac strip turns blue, it means it’s positive for blood. Give calcium gluconate for low Ca levels after the 3rd transfusion Hyperkalemia: low or high pulse rate, tall t waves, the pt be restless and weak Initially: Normal Hemoglobin Hematocrit Later: Decreased WBC Mild elevation Stool Guaiac for Occult blood Liver Enzymes Elevated in liver disease Electrolytes Watch Ca++ and K+ levels with blood replacement BUN Increased Diagnostic Procedures (don’t focus on these, just be aware) o Endoscopy Patient must be hemodynamically stable Area to be visualized should be cleared of blood o Tagged RBC or angiogram Done if endoscopy fails to identify source of bleeding o Wireless Capsule Endoscopy Can evaluate the areas of the small intestine Management o Control/Stop Bleeding Procedures for bleeding in PUD Endoscopic thermal therapy Endoscopic injection therapy o Injecting NS theory behind it is that it puts so much pressure on the vessels it occludes it and it stops bleeding Vagotomy and pyloroplasty o Vagotomy means they cut the vagas nerve, to stop the production of acetylcholine Procedures for bleeding in SRES Intraarterial injection Total gastrectomy Oversew ulcers Medications for bleeding in Varices Somatostatin (GHI) / Octreotide (Sandostatin): Used in combination to reduce portal HTN Vasopressin (Pitressin): Constricts splanchnic arterial bed reducing portal HTN Beta blockers: Reduce portal HTN - Prophylactic treatment of varices; *Not for Acute Bleeding Balloon Tamponade High risk of airway compromise Occlusion/Aspiration Gastric Perforation o Medical Emergency o Sudden, severe, generalized abdominal pain, rebound tenderness and rigidity Remember abd rigidity o Fever, leukocytosis, persistent tachycardia Stabilization o IV fluids: Crystalloids, Blood, Blood products Hb: 7 gm/dL & Hct: 21% How many units of PRBC would be needed to raise the client’s Hb to 9 gm/dL & Hct to 27%? 2 units of PRBC : Hb 9 gm/dL & Hct: 27%. o Central line o Supplemental oxygen o Intubation: Decrease risk for aspiration o Large-bore NG tube: Gastric lavage o Urinary catheter: Monitor urine output o Notes from bottom of slide Give IV fluids first! The bleeding is the problem, not the lack of O2. You’ll eventually give them O2, but they must be fluid resuscitated first If a person has esophageal varices, you don’t necessarily want to put an NG tube in, but you have to because you have to get the blood out of their gut. Gastric lavage: the dr will tell you to lavage til clear with room temp water. They used to use ice water to do this because of the vasoconstriction properties of the cold. But that does something about making them alkalotic (shift to the left, which is bad). All the vessels constrict, but the constricted cells don’t use oxygen as easily. Prophylactic and Treatment o Antacids - (1-3 hrs after meals and bedtime) Work on pH o Helicobacter pylori - (PUD, SRES) Antibiotics - Amoxicillin, Flagyl, Tetracycline Work on bacteria causing the problem o H2 Receptor Antagonists Tagamet, Pepcid, Zantac Work on reducing production of acid o Proton Pump Inhibitors - (Parietal Cells) Protonix, Nexium, Prilosec Slow the transport of HCl down o Prostaglandin E - (Mucous Cells) Cytotec (Increases HCO3, mucous) Carafate (Gastric acid Barrier) Work on mucous cells, increasing bicarb Nursing Management o Assess Gastric Fluid: pH monitoring: keep pH > 4 Litmus paper or direct NG tube probes o Monitor: Presence of bright-red or coffee-ground emesis. Bloody NG aspirate. Bright-red, black, or dark-red stools o Gastric Lavage: Large-bore NG tube. Irrigate (“Clear” return solution) Water vs. Normal saline Room temperature solutions vs. ice cold solutions Document amount instilled and aspirated