Respiratory System - El Camino College
advertisement

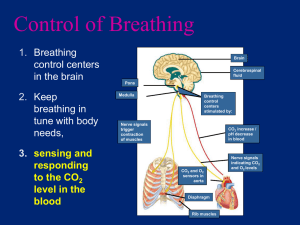
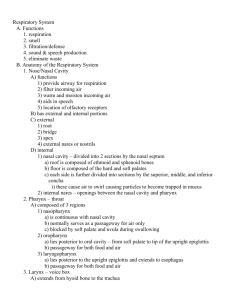
Anatomy & Physiology 34B Chapter 22 - Respiratory System I. Overview A. Introduction B. Conducting Passages C. Pulmonary Alveoli, Lungs, & Pleurae D. Mechanics of Ventilation E. Neural Control of Ventilation F. Gas Exchange & Transport G. Blood Chemistry and Respiratory Rhythm H. Respiratory Disorders II. Introduction to the _______________ System A. The major role of this system is to supply body tissues with ___________ and dispose of ____________________ (gas exchange) B. _______________ refers to 4 main functions: 1. Pulmonary _______________ - breathing 2. ___________ respiration - gas exchanges between the air & blood at the lung alveoli 3. _______________ of respiratory gases via the circulatory system 4. _____________ respiration – gas exchange between tissues & capillaries C. The respiratory system can be divided _____________ into upper & lower divisions, and __________________ into a conducting & a respiratory division D. Basic _______________ of the Respiratory System 1. Major passages & structures of the respiratory system are the a. ___________ respiratory - nasal cavity, pharynx, larynx, and trachea superior to the lungs b. __________ respiratory - bronchi, bronchioles, and pulmonary alveoli within the lungs 2. Air passes from nasal cavity pharynx larynx ____________ bronchi bronchioles _____________ 3. The _______________ division includes all the cavities and structures that transport gases to & from the pulmonary alveoli 4. The ___________ division consists of the pulmonary ______, which are the functional units of the respiratory system, where gas exchange between the air and blood occur III. _____________ Passages - transport air to the lungs; passages are lined with __________ that cleanse, warm, and humidify the air A. Nose - includes an external portion, the external _______, that opens to an internal nasal cavity, the nasal ___________ 1. The nasal _________ is formed by the following skull bones 2 a. b. Roof - frontal & _______ bones c. d. Posteriorly - __________ bone e. Medially – the nasal ________ formed by the perpendicular plate of the ethmoid, vomer, & septal cartilage Floor – ______ palate, formed by the palatine & maxillary bones, and muscular ______ palate Lateral walls have 3 bony projections: the superior, middle, and inferior nasal __________ (turbinates) 2. The conchae are lined with _________________ ciliated columnar epithelium that contain mucus-secreting __________ cells 3. 4. Nasal hairs (___________) in the nostrils filter inhaled macroparticles The main function of the nasal cavity is to _____, moisten, and filter the inspired air a. Debris from air is trapped in the _______ b. _________ move the mucus to the pharynx, where it is swallowed 5. ____________ is an inflammation of the nasal mucosa. B. ____________ Sinuses - communicate with the nasal cavity via drainage ducts. These paired sinuses include the FEMS: 1. 2. 3. 4. 5. ____________ ____________ _____________ _____________ _______________ is an inflammation of these sinuses. C. ______________ (throat) is divided into 3 regions: 1. ______pharynx - uppermost pharynx, behind the nasal cavity and above the soft palate; contains the 2. 3. a. _________ - hangs from the middle part of the soft palate; both block the nasal cavity during swallowing b. c. _____________ tubes - connect the nasopharynx with the middle ear cavities Pharyngeal tonsils (________) are found in the posterior wall of the nasal cavity ____pharynx - mid-pharynx between the soft palate and hyoid bone; contains paired a. ____________ tonsils on the posterior lateral wall; often become infected and are removed during a tonsilectomy b. Lingual tonsils on the base of the _________ _____________pharynx - posterior pharynx extends downward from the hyoid bone and opens into the esophagus & larynx. a. Food goes into the _______________ b. Air moves through the ___________ into the larynx and trachea 3 D. ____________ (“voice box”) - in anterior midline of the neck at C4-C6 1. The larynx prevents food from entering the ___________ and produces sound 2. It is composed of 9 ____________: 3 large unpaired and 6 smaller paired structures a. _________ cartilage - large, unpaired, anterior structure with a laryngeal prominence (________ apple) 3. b. _______________ - composed of elastic cartilage, located behind the root of the tongue; during swallowing, it folds over the _________ opening to the larynx c. ___________ cartilage - ring shaped base of larynx; connects thyroid cartilage to the trachea d. _________ cartilages - paired above the cricoid and behind the thyroid; posterior attachments of the vocal folds e. _____________ & corniculate cartilages - paired, small accessory structures associated with the arytenoid cartilages Two pairs of strong CT bands are stretched between the thyroid & __________ cartilages a. b. 4. ________ folds (true vocal cords) - vibrate to produce sound ___________ folds (false vocal cords) - support the vocal folds, but do not produce sound Laryngeal _____________ include a. b. ______________ muscles - elevate the larynx during swallowing ____________ muscles - change length, position, & tension of the vocal folds 5. _____________ is an inflammation of the larynx E. ______________ (windpipe) 1. Rigid tube anterior to the __________; connects the larynx to the primary bronchi 2. 16-20 anterior hyaline cartilage _________ form the supporting walls of the trachea 3. The trachea mucosal lining consists of ____________________ ciliated columnar epithelium with many goblet cells; this moves particles out of the lungs 4. Medial to the lungs, the trachea splits at the ______ to form the left and right primary bronchi F. _________ ________ - respiratory tubes branch into progressively narrower tubes as they extend into the lungs in the following order: 1. 2. 3. 4. 5. 6. 7. L. & R. ____________ bronchi ____________ (lobular) bronchi ____________ (segmental) bronchi ______________ ______________ bronchioles ______________ bronchioles Alveolar _______ 4 8. 9. Alveolar _____ Pulmonary ____________ G. The ___________ portion ends at the terminal bronchioles and the ___________ portion begins at the respiratory bronchioles IV. Pulmonary Alveoli, Lungs, & Pluera A. Pulmonary Alveoli 1. Alveolar sacs are clusters of tiny pulmonary __________, the functional units of the respiratory system. Alveolar _____ are a. Type I – simple ___________ epithelium surrounded by a basal lamina, forming a thin ______________________ shared by alveoli and surrounding capillaries b. Type II – ___________ epithelium that secretes lubricating ______________ that keeps alveoli from sticking together c. Alveolar _______________ that phagocytize pathogens 2. Gas exchange occurs across the respiratory _____________ between the alveoli and their associated capillaries a. b. ___________ diffuses across the alveoli walls into the capillaries __________ diffuses from the capillaries into the alveoli B. ______ - paired respiratory organs lateral to the mediastinum and surrounded by the rib cage within the thoracic cavity 1. 2. Each lung has 4 surfaces: a. ______________ (medial) surface - slightly concave and contains a verticle slit, the hilum through which pulmonary vessels, nerves, & bronchi pass b. c. d. ______ - concave inferior surface that fits over the diaphragm ______ - pointed, superior surface that extends above the clavicle ___________ surface - rounded lateral surface in contact with the membranes covering the lungs Right & left lungs are similar, but have some differences: a. Left lung has a ________ notch on its medial surface and is divided by a ______ fissure into a superior and inferior lobe b. c. Right lung is divided by ____ fissures into superior, middle, and inferior lobes. Each lobe is further divided into many smaller ___________, which contain the pulmonary alveoli C. _________ - serous membranes that surround the lungs and line the thoracic cavity include the 1. ___________ pleura adheres to the outer lung surface and extends into the interlobular fissures 2. ___________ pleura lines the thoracic cavity and the mediastinum, thus both lungs are in separate compartments 5 3. A pleural _______ is a potential space between the visceral & parietal pleura; pleural fluid in this cavity allows the membranes to slide smoothly across each other during respiration 4. ____________ is an inflammation of the pleura, which causes friction between lungs and thoracic cavity, making breathing difficult V. Mechanics of Ventilation A. Pulmonary _____________ (breathing) consists of two phases: inspiration (inhaling) and expiration (exhaling) B. Relaxed ___________ involves contractions of the diaphragm and external intercostal muscles 1. Contraction of the dome-shaped _______ causes it to flatten, increasing lung volume; contractions of the external intercostals lift the ribs, further increasing lung volume a. _________ Law – the pressure of a quantity of gas is inversely proportional to the volume of its container (P1/V) b. During inspiration alveolar volume increases, which __________ intrapulmonary pressure below atmospheric pressure (760 mm Hg 757 mm Hg) c. In terms of ________ pressure, if atmospheric pressure was 0, the intrapulmonary pressure would be –3 mm Hg; thus air flows _____ the lungs d. Intrapleural pressure (-4 -6 mm Hg) is the pressure in the __________ cavity, which is always more negative than the intrapulmonary pressure, and acts as a suction to keep lungs inflated e. Transpulmonary pressure is the difference between the intrapulmonary and _____________ pressures (757 754 mm Hg); this helps the lungs to expand in the thoracic cavity 2. Nerves involved include the __________, intercostal, accessory, cervical, & thoracic nerves C. Forced inspiration involves contractions of the ___________ and sternocleidomastoid muscles, which further elevate the ribs D. Relaxed __________ - muscles of inspiration relax, ribs return to their original position, elastic tissue in the lungs and bronchial tree allow them to recoil 1. Lung internal volume decreases, causing intrapulmonary pressure to ____________ 2. Intrapulmonary pressure becomes +3 mm Hg above atmospheric pressure, so air flows _____ of the lungs E. During forced expiration, internal intercostals and _____________ muscles contract in response to intercostal and lower spinal nerves F. Other factors affecting respiration include resistance to airflow, alvoelar surface tension, and alveolar ventilation 1. _____________ to airflow within airways is affected by pulmonary compliance and bronchiole diameter (F Pressure/Resistance) a. Pulmonary __________, the ease with which the lungs expand, can be reduced by lung diseases that increase resistance, thus decreasing air flow b. Changes in bronchiole ____________ affect resistance 6 1) Bronchoconstriction occurs when parasympathetic nerves or histamine _______ bronchioles, leading to increased resistance and ______________ air flow 2) Bronchodilation occurs when epinephrine, released by the adrenal gland during exercise or stress, _________ bronchioles, leading to decreased resistance and ____________ air flow 2. Alveolar ____________________ is reduced by surfactant a. Surfactant is a lipoprotein produced by type ___ alveolar cells; it reduces alveolar surface tension, allowing the alveoli to recoil during expiration b. Premature infants are often deficient in surfactant, which causes hyaline membrane disease (Respiratory ____________ Syndrome) 3. Alveolar ventilation is limited by the amount of air that reaches functional ________ a. The conducting division of the respiratory system is called anatomical _________ because air here is not involved in gas exchange b. _______________ dead space is the sum of the anatomical dead space and pathological alveolar dead space c. Alveolar ________________ is determined by taking the difference of the inhaled air (500 ml) minus the dead air (150 ml), then multiplying the result by the respiratory rate (BPM) G. Measurements of Ventilation can be obtained via a ______________, which captures expired air and records the rate and depth of breathing, speed of expiration, and rate of oxygen consumption. Measurements are respiratory volumes or respiratory capacities 1. ________ volume (TV) - amount of air inhaled or exhaled in one respiratory cycle (500 mL) 2. _____________reserve volume (IRV) – amount of air above the tidal volume that can be inhaled with maximum effort (3,000 mL) 3. ______________reserve volume (ERV) – amount of air above the tidal volume that can be exhaled with maximum effort (1,200 mL) 4. ____________ volume (RV) – amount of air left in lungs after maximum expiration (1,300 mL) 5. _________________ – amount of air that can be exhaled with maximum effort after maximum inspiration (VC = TV + IRV + ERV) (4,700 mL) 6. _________ expiratory volume (FEV) – percent of the vital capacity that can be exhaled in a given time interval. 1) Healthy adults should be able to expel 75-85% of the vital ___________ in one second. 2) Inability to do so may indicate respiratory ____________ VI. Neural Control of Ventilation A. The three ___________ _____________ of the brain are the 1. ______________ area in the medulla oblongata contains nerve cell bodies that form the inspiratory and expiratory portions a. Inspiratory (I) neurons fire during _____________ b. Expiratory (E) neurons fire during forced ____________ 2. Apneustic & pneumotaxic areas in the _____ influence the activity of the rhythmicity area 7 a. b. ______________ center prolongs inspiration ___________________ center inhibits medullary inspiratory neurons B. Excessive inflation in the lungs triggers the Hering-Breuer _______, in which inspiratory neurons are inhibited and expiration results C. Breathing can be voluntarily controlled to a point. Holding one’s breath lowers the ___ level and raises the ____ level in the blood until autonomic controls force the person to breath VII. Gas Exchange & Transport A. Air is a mixture of ______: 78.6% N2, 20.9% O2, 0.46% H20, and 0.04% CO2 (note that alveolar air differs in percentages) 1. Each gas contributes a ________ ___________ to the total atmospheric pressure in proportion to its percentage (e.g., Patm = PN2 + PO2 + PH2O + PCO2 = 597 + 159 + 3.7 + 0.3 = 760 mm Hg) 2. ____________ Law – the total pressure of a gas mixture is the sum of the partial pressures of the individual gases 3. Partial gas pressures are important because they determine the rate of _____________ of a gas, and thus affect the rate of gas exchange between the blood and alveolar air B. At the Air-Water Interface (as in the pulmonary alveolus), gases diffuse down their concentration gradients until __________________ is reached 1. ____________ Law – the amount of gas that dissolves in a liquid is proportional to a. the partial ____________ of the gas and b. the _____________ of the gas C. Gas ___________ – the process of carrying gases from the alveoli to the systemic tissues and back 1. ________ transport is accomplished mainly by O2 binding to ___ (98.5%), with a slight percentage dissolved in the plasma (1.5%) a. At high PO2 (as in the lungs), Hb has a ___ _______ for O2; the iron in each of the 4 heme groups binds one O2 molecule, and Hb becomes oxyhemoglobin (_____) b. At low PO2 (as in the tissues), Hb has a ______________ for O2, so the heme groups release the O2 to diffuse out to the tissues. Once the O2 is released, the Hb becomes _______hemoglobin c. Hb has a higher affinity for ____ than it does for O2, so if CO is present, it will competitively bind to Hb, preventing ____ from binding, which can lead to death 2. Carbon _______ transport is accomplished in three ways: as carbonic acid, carbamino compounds, and dissolved gas a. About 70% of CO2 reacts with water to form carbonic acid (________), which then dissociates into bicarbonate (______) and hydrogen ions (__) in RBCs. This rxn. is facilitated by the enzyme carbonic anhydrase (____) CO2 + H2O H2CO3 HCO3- + H+ CAH b. About 23% of CO2 binds with hemoglobin to form carbaminohemoglobin (______). CO2 does not compete with O2 because they bind to different sites on Hb. c. The remaining 7% of CO2 is carried in blood ________ as a dissolved gas, like the CO2 in soda pop (note: CAH is present in RBCs, but not in plasma) 8 D. ____________ Gas Exchange is the unloading of O2 and loading of CO2 at the systemic capillaries in tissues 1. CO2 loading – CO2 is a by product of cellular __________ in tissues, therefore PCO2 is higher in tissues than in capillaries, thus CO2 diffuses ____ the bloodstream 2. Oxygen unloading- __________ ions dissociated from carbonic acid bind to ____hemoglobin, which reduces Hb’s affinity for O2, causing the release of O2, which diffuses to surrounding tissues E. ___________ gas exchange is the loading of O2 and unloading of CO2 at the alveolar capillaries 1. More PO2 in alveolar air than in capillary blood allows O2 to diffuse into the _______ (O2 loading) a. As Hb loads O2, its affinity for ____ declines b. Hydrogen ions dissociate from Hb and bind with ___________ ions transported from the plasma into RBCs c. The reaction of H+ and HCO3- reverses the previous hydration rxn. and generates free _____ 2. Greater PCO2 in the capillary blood than in the alveolus allows CO2 to diffuse into the ____________ (CO2 unloading) 3. Even though PO2 is CO2, equal amounts of O2 and CO2 are exchanged across the respiratory membrane because CO2 is much more ___________ than O2 F. Adjustment to Changing Metabolic Needs of Tissues 1. Four factors adjust the rate of ____ unloading a. Ambient O2 - Active tissues consume O2 rapidly, leading to a ________ PO2 than resting tissues, thus HbO2 releases more O2 to active tissues b. ___________ – elevated temperature in active tissues also promotes O2 unloading c. Bohr effect – active tissues generate extra CO2, which raises the ___ concentration and lowers blood ___; this also promotes O2 unloading d. Bisphosphoglycerate (___), an enzyme in anerobic respiration in RBCs, binds to Hb and promotes O2 unloading 2. CO2 loading is affected by a low level of _____, which enables Hb to transport more CO2 (the Haldane effect) VIII. Blood Chemistry & Respiratory Rhythm A. Two groups of ___________________ respond to changes in blood chemistry 1. ___________ chemoreceptors in the MO monitor the ___ of the CSF and tissue fluid of the brain 2. _______________ chemoreceptors in the aortic and carotid bodies a. b. Aortic bodies in the _______ arch send sensory information to the MO in the __________ nerves Carotid bodies in the ___________ arteries stimulate sensory fibers in the glossopharyngeal nerve B. Effects of hydrogen ions, O2 and CO2 concentrations on respiration 1. Hydrogen ion concentration (___) in the brain is controlled mainly by ventilation a. Blood pH is determined largely by _____ because of the rxn. CO2 + H2O H2CO3 HCO3- + H+ 9 b. The more CO2 is present, the more H+ is generated, the lower the pH; less CO2 = _____ H+ ions = _________ pH c. Blood pH must be maintained within a narrow range of 7.35-7.45; lower is called ___________, higher is ___________ d. Respiratory acidosis is usually caused by excess CO2 (____________), which can be corrected by _____________ ventilation to expel more CO2 e. Respiratory alkalosis is usually caused by low CO2 (_____________), which can be corrected by ____________ ventilation to allow CO2 to build up in the blood 2. Carbon dioxide – at the beginning of exercise, rising ___ levels stimulate peripheral chemoreceptors, which trigger an ______________ in ventilation 3. Oxygen – PO2 usually has little effect on ventilation, but long term _____________ (as in emphysema and mountain climbing) can trigger ____________ drive, in which ventilation is increased IX. Respiratory Disorders A. ____________, a deficiency of O2 in the tissues, can cause cyanosis and, if severe and prolonged, can lead to tissue necrosis B. Trauma or Injury Problems 1. _____________ is a condition in which the lung(s) collapse (atelectasis) if air enters the pleural cavity. 2. ___________ - foreign object lodges in the trachea; may be dislodged by the ____________ maneuver C. Chronic obstructive pulmonary diseases (_________s) 1. _____________ - acute infection & inflammation of the lung accompanied by fluid buildup; may be caused by bacteria, virus, or fungus 2. ________________ - inflammatory lung disease contracted by inhaling tuberculosis bacteria from a carrier 3. ____________ - caused by allergy to inhaled antigens; causes a swelling or blockage of lower respiratory tubes 4. Chronic ___________ – often found in smokers, tobacco smoke paralyzes and eventually destroys cilia and alveolar macrophages; excess mucus production leads to coughing and infection 5. ________________ - causes the breakdown of the pulmonary alveoli, increasing the size of air spaces and decreasing their surface area and respiration; frequent cause of death among smokers. D. __________________, which causes 1/3 of all cancer deaths in the U.S., is caused mostly by tobacco smoke, which contains numerous carcinogenic compounds 1. Three forms of lung cancer are ________ cell carcinoma, _____carcinoma, and ________________ carcinoma 2. Symptoms include chronic coughing and ________ in the sputum 3. Lung cancer ______________ so rapidly, it has usually spread to other organs by the time it is diagnosed, and prognosis is poor