Chapter 11
advertisement
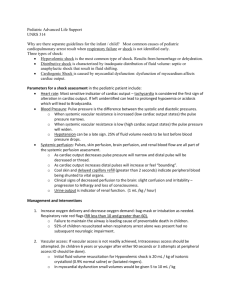
Ready for Review Perfusion is the circulation of blood within an organ or tissue in adequate amounts to meet the cells’ current needs for oxygen, nutrients, and waste removal. Perfusion requires an intact cardiovascular system and a functioning respiratory system. Blood is the vehicle for carrying oxygen and nutrients through the vessels to the capillary beds to tissue cells, where these supplies are exchanged for waste products. Blood flow through the capillary beds is regulated by the capillary sphincters that are under the control of the autonomic nervous system. Regulation of blood flow occurs by vessel constriction or dilation, along with sphincter constriction or dilation. The systolic pressure is the peak arterial pressure, or pressure generated every time the heart contracts; the diastolic pressure is the pressure maintained within the arteries while the heart rests between heartbeats. Perfusion depends on cardiac output, systemic vascular resistance (SVR), and transport of oxygen. Cardiac output (CO) is the volume of blood that the heart can pump per minute. Systemic vascular resistance is the resistance to blood flow within all of the blood vessels except the pulmonary vessels. Most types of shock (hypoperfusion) are caused by dysfunction in one or more parts of the perfusion triangle: – The pump (the heart) – The pipes, or container (blood vessels) – The content, or volume (blood) Shock (hypoperfusion) is the collapse and failure of the cardiovascular system, when blood circulation slows and eventually stops. The body has neural and hormonal mechanisms for regulating blood pressure. Maintenance of blood pressure is important to maintaining homeostasis. If perfusion decreases, baroreceptors sense the decreased flow and activate the vasomotor center, which oversees changes in the diameter of blood vessels, to begin constriction of the vessels and increase blood pressure. Chemoreceptors are stimulated by decreases in PaO2 and increases in PaCO2 and are important in regulating respiration. Failure of compensatory mechanisms to preserve perfusion leads to decreases in preload and cardiac output. Myocardial blood supply and oxygenation decrease, reducing myocardial perfusion. As cardiac output further decreases, coronary artery perfusion also decreases, leading to myocardial ischemia. Multiple-organ dysfunction syndrome (MODS) is a progressive condition in which several organs fail. This occurs when injury or infection triggers a massive systemic immune, inflammatory, and coagulation response. The various types of shock are cardiogenic, obstructive, septic, neurogenic, anaphylactic, psychogenic, and hypovolemic. Signs of compensated shock include anxiety or agitation; tachycardia; pale, cool, moist skin; increased respiratory rate; nausea and vomiting; and increased thirst. If there is any question on your part, treat for shock. It is never wrong to treat for shock. Signs of decompensated shock include labored or irregular respirations, ashen gray or cyanotic skin color, weak or absent distal pulses, dilated pupils, and profound hypotension. Irreversible shock is the terminal stage. Even aggressive treatment at this stage does not usually result in recovery. Remember, by the time a drop in blood pressure is detected, shock is usually in an advanced stage. Anticipate shock in patients who may have the following conditions: – Severe infection – Significant blunt force trauma or penetrating trauma – Massive external bleeding or index of suspicion for major internal bleeding – Spinal injury – Chest or abdominal injury – Major heart attack – Anaphylaxis Treating a pediatric or geriatric patient in shock is no different than treating any other shock patient. Treat all patients suspected to be in shock from any cause as follows and in this order: – Open and maintain the airway. If cardiac arrest is suspected, focus on high-quality chest compressions prior to airway and breathing. – Provide high-flow oxygen and, as needed, provide bag-mask assisted ventilations. – Control all obvious external bleeding. – Place the patient in the shock position or, if on a backboard or stretcher, elevate the end of the board. – Maintain normal body temperature with blankets. – Provide prompt transport to the appropriate hospital. – Gain IV access. Starting an IV and administering fluids is part of treating a patient who is in shock. Administer IV volume expanders (warmed if possible) to replace blood loss. Isotonic crystalloids, such as normal saline or lactated Ringer’s, should be used (synthetic solutions may also be used). Call early for paramedic intervention to administer vasopressors if needed.




![Electrical Safety[]](http://s2.studylib.net/store/data/005402709_1-78da758a33a77d446a45dc5dd76faacd-300x300.png)