Pediatric Advanced Life Support
advertisement

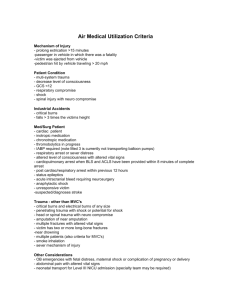
Pediatric Advanced Life Support UNRS 314 Why are there separate guidelines for the infant / child? Most common causes of pediatric cardiopulmonary arrest result when respiratory failure or shock is not identified early. Three types of shock: Hypovolemic shock is the most common type of shock. Results from hemorrhage or dehydration. Distributive shock is characterized by inadequate distribution of fluid volume: septic or anaphylactic shock that result in fluid shifting. Cardiogenic Shock is caused by myocardial dysfunction: dysfunction of myocardium affects cardiac output. Parameters for a shock assessment in the pediatric patient include: Heart rate: Most sensitive indicator of cardiac output – tachycardia is considered the first sign of alteration in cardiac output. If left unidentified can lead to prolonged hypoxemia or acidosis which will lead to Bradycardia. Blood Pressure: Pulse pressure is the difference between the systolic and diastolic pressures. o When systemic vascular resistance is increased (low cardiac output states) the pulse pressure narrows. o When systemic vascular resistance is low (high cardiac output states) the pulse pressure will widen. o Hypotension can be a late sign. 25% of fluid volume needs to be lost before blood pressure drops. Systemic perfusion: Pulses, skin perfusion, brain perfusion, and renal blood flow are all part of the systemic perfusion assessment. o As cardiac output decreases pulse pressure will narrow and distal pulse will be decreased or thread. o As cardiac output increases distal pulses will increase or feel “bounding”. o Cool skin and delayed capillary refill (greater than 2 seconds) indicate peripheral blood being shunted to vital organs. o Clinical signs of decreased perfusion to the brain: slight confusion and irritability – progression to lethargy and loss of consciousness. o Urine output is indicator of renal function. (1 mL /kg / hour) Management and Interventions 1. Increase oxygen delivery and decrease oxygen demand: bag-mask or intubation as needed. Respiratory rate red flags (RR less than 10 and greater than 60). o Failure to maintain the airway is leading cause of preventable death in children. o 92% of children resuscitated when respiratory arrest alone was present had no subsequent neurologic impairment. 2. Vascular access: If vascular access is not readily achieved, Intraosseous access should be attempted. (In children 6 years or younger after either 90 seconds or 3 attempts at peripheral access IO should be done). o Initial fluid volume resuscitation for Hypovolemic shock is 20 mL / kg of isotonic crystalloid (0.9% normal saline) or (lactated ringers). o In myocardial dysfunction small volumes would be given 5 to 10 mL / kg 3. Drugs used in Cardiac Resuscitation: o o o o Epinephrine: (classification: inotropic agent): primary drug for treating patients with cardiopulmonary arrest. Actions: stimulates a-adrenergic receptors, increases SVR (constriction of arterioles) increases diastolic blood pressure; stimulates B2 adrenergic receptors (increases heart rate); Increases myocardial contractility Dosing IV or IO: 0.01 mg per kg 1:10,000. Bradycardia is the most common dysrhythmia in the pediatric population – epinephrine drug of choice. Asystole: epinephrine would be drug of choice. Adenosine: (classification: antiarrhythmic) Indication: SVT. Action: stimulates adenosine receptors in heart and vascular smooth muscle. Briefly blocks the conduction through AV node. Allows return of normal sinus rhythm in patients with SVT, including SVT associated with WolffParkinson-White Syndrome. Depresses sinus node automaticity. Pharmocodynamics: onset – rapid, peak – unknown, duration – usually less than a minute. Nursing considerations: record rhythm strip during administration. Administer via central venous access if possible, otherwise IV / IO in most proximal site. Push rapidly followed immediately by NS flush (5 to 10 mL). Amiodarone: (classification: antiarrhythmic). Has both Alpha and Beta adrenergic antagonist effects: primary drug to be used in ventricular fibrillation and ventricular tachycardia. Used in Pulseless arrest after Epinephrine. Actions: prolongs action potential duration and effective refractory period, slows sinus rate, prolongs PR and QT intervals Pharmocodynamics: onset – within hours, peak – 2-3 days, duration – 2 weeks to months after stopping drug Dosing is 5 mg / kg over 20 minutes can be repeated as necessary. Special considerations: because of the long half-life and potential drug interaction, consultation with cardiologist is encouraged Albuterol: (classification: bronchodilator, B2-adrenergic agent. Indications: asthma, anaphylaxis (bronchospasm) and hyperkalemia. Action: Stimulates B2-adrenergic receptors, causing bronchodilation, tachycardia, vasodilatation, movement of potassium from extracellular to intracellular space (serum potassium will fall). Given via nebulized solution: 0.5 % (5mg/mL) 4. Automated External Defibrillator Guidelines: 85% of children in cardiac arrest are due to asystole or Pulseless electrical activity. AHA is recommending that automated external defibrillators be used in children with sudden collapse or presumed cardiac arrest. 2 J per kg to 4 J per kg. 5. Inotropic drugs used to manage children status post resuscitation: o o o Epinephrine (continuous infusion) bradycardia, shock and hypotension Dopamine used in treatment of hypotension and shock in the presence of adequate intravascular volume. Classification: catecholamine, vasopressor, inotrope. Indications: cardiogenic or distributive shock. Actions: Stimulates a-adrenergic receptors (increases VR via constriction of arterioles; stimulates B1-adrenergic receptors (increases heart rate- SA node), stimulates B2-adrenergic receptors: increases HR Pharmocodynamics: onset – 1-2 minutes, peak – 10 minutes, duration: < 10 minutes when infusion stopped Continuous infusion Dobutamine: Classification: catecholamine, B-adrenergic agent. Indications: congestive heart failure and Cardiogenic shock. Actions: stimulates B1-receptors increases heart rate, SA node effect; stimulates B2-receptors, which increases heart rate and causes vasodilation. Pharmocodynamics: onset – 1-2 minutes, peak – 10 minutes, duration - < 10 minutes when infusion stopped Nursing responsibilities: monitor BP and ECG continuously