Shock
advertisement

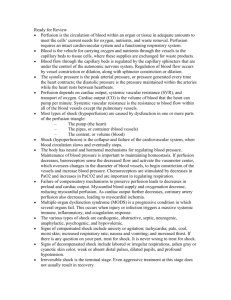
Diagnosis and Management of Shock Dr. Anas Khan Consultant, EM MBBS, MHA, ArBEM 428 C2 notes Objectives Identify the 4 main categories of shock. Discuss the goals of resuscitation in shock. Summarize the general principles of shock management. Describe the physiologic effects of vasopressors and inotropic agents. CASE STUDY A 25 Years old lady, with no prior history of any chronic disease, presented to the emergency department C/O productive cough of greenish yellow sputum. V/S Temp: 38.8 ( each 1o C higher in temperature must have an increase in HR by 10-15 beats, here after calculations HR is still higher then it should be (115). HR: 129 /Min (60-100/min) R.R: 27 /Min ( 16-20/min) BP: 112/68 Questions Where do you triage this Pt.? Triage : to prioritize the patients Information we still have to collect to be able to classify the patient : condition of patient , if in distress, check vitals BP,HR,RR,temperature,oxygen saturation,glucocheck if the patient is dizzy What information do you need to determine if this Pt. is in shock? What initial interventions are needed to stabilize that Pt.? Shock Shock is a syndrome of impaired tissue oxygenation and perfusion due to a variety of etiologies that will result in different manifestations according to organ affected. Liver --- nausea/vomiting Heart --- tachycardia Lung --- SOB Brain --- confusion kidney --- oliguria and late stage anuria If left untreated - Irreversible injury - Organ dysfunction - Death Clinical Alterations in Shock The presentation of patients with shock may be subtle (mild confusion, tachycardia). Or easily identifiable (profound hypotension, anuria) Pathophysiology: 1- Inadequate tissue perfusion and oxygenation 2- Compensatory responses 3- The specific etiology --- you should manage the patient but must aim to treat the underlying cause. Classification 1- Hypovolemic: (hemorrhagic (internal as bleeding ulcers or external as acute blood loss), non-hemorrhagic ( dehydration as vomiting and diarrhea,3rd fluid spacing as in burns and pancreatitis). 2- Cardiogenic: pump related, any type of cardiomyopathies (ischemic, myopathy, mechanical, arrhythmogenic either braycardic or tachycardia). 3- Distributive: mainly due to vasodilation (septic, adrenal crises due to steroids withdrawal mostly iatrogenic, neurogenic loss of sympathetic tone when there is trauma to the thoracic or lumbar sympathetic chain or spinal cord injury, anaphylactic as in hypersensitivity reactions if severe form). 4- Obstructive: (massive PE, tension pneumothorax(space is obstructed by fluid), cardiac tamponade( space is obstructed with blood, constrictive pericarditis(space is obstructed due to the inflammation.) *spinal shock is different from neurogenic , its just motor loss which is transient and due to concussion, no vascular changes so not considered as an ER shock X-ray of tension pneumothorax which is an immediate ER. CT of pulmonary embolism Hypovolemic Shock When the IV volume is depleted relative to the vascular capacity as a result of: 1- Hemorrhage. 2- GI loss 3- Urinary loss 4- Dehydration Hypovolemic Shock Management - The goal is to restore the fluid lost - Vasopressors are used only as a temporary method to restore B.P until fluid resuscitation take place * Mainly we give good volume of fluids to prevent heart failure . Vasopressors has no role . Distributive shock It is characterized by loss of vascular tone. The most common form of distributive shock is septic shock. Hemodynamic Profile Cardiac output normal or increased Ventricular filing pressure normal or low SVR low Diastolic pressure low Pulse pressure wide Management of Septic Shock The initial approach to the patient with septic shock is the restoration and maintenance of adequate intravascular volume. * If not maintained by fluids we give vasopressors unlike hypovolemic shock . Prompt institution of appropriate antibiotic. * In each 1 hour delay in antibiotics initiation will increase 6.7% mortality . Cardiogenic Shock Forward flow of blood is inadequate because of pump failure due to loss of functional myocardium. It is the most severe form of heart failure and it is distinguished from chronic heart failure by the presence of: - hypotension, hypo perfusion and the need for different therapeutic interventions. Hemodynamic Profile: Cardiac output Ventricular filing pressure * Venous return SVR *systemic vascular resistance Mixed venous O2 sat Low Low High High Management of Cardiogenic Shock The main goal is to improve myocardial function. Arrhythmia should be treated. Reperfusion PCI is the treatment of choice in ACS. * Percutaneous Coronary Intervention standard of care , should be started within 90 minutes window if not then go for thrombolytic agents . Inotropes and vasopressors. Obstructive Shock Obstruction to the outflow due to impaired cardiac filling and excessive after-load Cardiac tamponade & constrictive pericarditis impair diastolic filling of the Rt. ventricle Tension pneumothorax obstructs venous return limiting Rt. ventricular filing. * In tension pneumothorax there is positive gradient pressure limiting venous return Massive pulmonary embolism increase the Rt. ventricular after-load. Hemodynamic Profile Cardiac output low Afterload * same as SVR (systemic venous return ) high Lt.Vent.filling pressure variable Pulsus paradoxicus (in Tamponade) * Pulsus paradoxicus normally with inspiration it increase by 10 beats if more then positive for temponade . Distended Jugular veins Management Of Obstructive Shock Directed Mainly to Management of the cause. General Principles The overall goal of shock management is to improve oxygen delivery or utilization in order to prevent cellular and organ injury. * Defect in utilization as in CO poising because hemoglobin has higher affinity to CO and even if one oxygen went there the CO will prevent the off-load and if it did at the mitochondrial level it wil block the respiratory chain . Effective therapy requires treatment of the underlying etiology. Restoration of adequate perfusion, monitoring and comprehensive supportive care. Interventions to restore perfusion center on achieving an adequate BP, increasing cardiac output and optimizing oxygen content of the blood (goal directed therapy). Oxygen demand should also be reduced. * Most important is 1- Brain , 2- Heart and 3- Diaphragm which take 30% of oxygen found in blood , mechanical ventilation in all this you should decrease demand . * Hyperdynamic state : Thryrotoxicosis , Anemia , Fever and late term pregnancy . In Summery, Shock Management: 1- Monitoring. 2- Fluid Therapy. 3- Vasoactive agents. 4- Treat the underlying cause. THANK YOU


![Electrical Safety[]](http://s2.studylib.net/store/data/005402709_1-78da758a33a77d446a45dc5dd76faacd-300x300.png)