DEVELOPMENT OF RESPIRATORY SYSTEM
advertisement

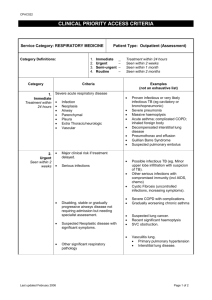
DEVELOPMENT OF RESPIRATORY SYSTEM AND ITS ANOMALIES LEARNING OBJECTIVES: 1. Enumerate the different Parts of Respiratory System 2. Name the Different Parts of Foregut 3. Discuss the formation of laryngo- tracheal tube 4. Discuss the formation of Lung Bud 5. Describe the Branches of Bronchi 6. Discuss the different Stages of development of Lung 7. Describe Maturation of Lung 8. Enumerate the congenital errors during development LECTURE OUTLINE DIFFERENTIATION (ORGANOGENESIS) • ORGanogenesis is the formation of the organs. Arises from the layering of cells that occurs during gastrula stage • The layers are germ layers; they have specific fates in the developing embryo: – Endoderm – Mesoderm – Ectoderm Differentiation of Primary Germ Layers (from the gastrula) Ectoderm Nervous system Mesoderm Skeleton Endoderm Digestive tract Epidermis of skin Muscles Respiratory system Circulatory system Liver, pancreas Gonads Bladder FUNCTIONAL DIVISION OF RESPIRATORY SYSTEM Functionally the Respiratory System is divided into two parts: Conducting Part Respiratory Part CONDUCTING PART: Nostrils Vestibule Nasal Cavity Nasopharynx Oropharynx Laryngopharynx Larynx, Trachea Principal Bronchi Secondary Bronchi Segmental Bronchi Upto Terminal Bronchioles RESPIRATORY PART Respiratory Bronchioles Alveolar Duct Alveolar Sac, Alveoli Developmental Division of Respiratory System Developmentally the Respiratory System is divided into two parts: 1. Upper Part of Respiratory System 2. Lower Part of Respiratory System Upper part of respiratory system Extends from nose to larynx Develops from the Pharyngeal Apparatus which is a part of Head & Neck Lower Part of Respiratory System Extends below the Larynx up to lung alveoli This part develops From the Foregut DEVELOPMENT OF THE NOSE Related to formation of face Nasal placodes- primordia of nose and nasal cavities Proliferation of mesenchyme in margins of nasal placode medial and lateral nasal prominences Nasal pit- primordia of nares and nasal cavities Medial nasal prominences form the tip of the nose, nasal septum, and the intermaxillary segment Lateral nasal prominences form the sides (alae) of the nose Frontonasal prominence forms the bridge of the nose LARYNX GERM LAYER ORIGIN Mesoderm- cartilages and muscles (4th & 6th pharyngeal arches, thyroid , cricoid and Arytenoid) Endoderm- internal lining of the epithelium Transformation of mesenchyme to cartilaginous components produces T shaped laryngeal orifice Epithelium- endoderm Thyroid, cricoid, arytenoid cartilages and muscles from 4th and 6th branchial arches Transformation of mesenchyme to cartilaginous components produces T shaped laryngeal orifice Different Parts of Foregut The foregut can be divided into three parts: 1. The first part lies ventral to the developing brain, and forms the primitive pharynx, which has the branchial arches associated with it. 2. The second part lies dorsal to the heart, and forms the lung bud and the oesophagus. 3. The third part lies dorsal to the septum transversum and forms the stomach and other related gastro-intestinal structures. Respiratory System is derived from Second Part of Foregut a. It begins to develop in the beginning of the fourth week (day 22) b. It begins as a laryngo- tracheal groove on the ventral aspect of the foregut, which deepens and forms a repiratory diverticulum. c. Separates from the oesophagus Development of Lung Bud The respiratory diverticulum's bifurcates into right and left bronchial buds on day 26-28. Division of Lung Bud Asymmetric branching occurs during the following 2 weeks to form secondary bronchi: 3 on the right and 2 on the left forming the main divisions of the bronchial tree. The lung bud and its subsequent branches are of endodermal origin. They give rise to the epithelium lining all the respiratory passages, the alveoli and the associated glands. The surrounding mesoderm, the splanchnopleure, gives rise to all the supporting structures: the connective tissue, cartilage, muscle and blood vessels. Branching of Bronchi The pattern of branching is regulated by the surrounding mesoderm. The mesoderm surrounding the trachea inhibits branching whereas the mesoderm surrounding the bronchi stimulates branching. Transplantation of part of the bronchial mesoderm to replace part of the tracheal mesoderm forms an ectopic lobe of the lung arising directly from the trachea. Transplantation of part of the tracheal mesoderm to replace part of the bronchial mesoderm suppresses the formation of a lobe. During weeks 7 to 16 branching occurs about 14 times to the level of terminal bronchioles. At this stage there are no alveoli. The foetal lung during this period is described as the glandular stage because the terminal bronchioles resemble glandular acini. The bronchi, containing cartilage in their walls, identify the sections as foetal lung. Stages of Development of the Lungs 1. The Pseudo-glandular stage – weeks 6 to 16 – there is repeated branching about 14 times) to the level of the terminal bronchioles. 2. The canalicular stage – weeks 16 to 26 – the respiratory bronchioles develop 3. The saccular stage – weeks 26 to 36 Development (the primary alveoli develop). 4. The alveolar stage – weeks 36 to 40 – the alveoli mature: Pseudoglandular phase (6 to 16 Weeks) At this stage the lungs resemble the development of a Exocrine Gland. By the end of 16 weeks all the major elements of the lung development have formed except those involved with gas exchange. Respiration is not possible, hence fetuses born during this period are unable to survive CANALICULAR PHASE In the classical description of lung development, in this phase the canaliculi branch out of the terminal bronchioli. The canaliculi compose the proper respiratory part of the lungs, the pulmonary parenchyma.. Alveolar phase Depending on the author, the alveolar phase begins at varying times. Probably in the last few weeks of the pregnancy, new sacculi and, from them, the first alveoli form. Thus, at birth,1/3 of the roughly 300 million alveoli should be fully developed. Maturation of Lung Characteristic mature alveoli do not form until after birth, about 95% of alveoli develop postnatally. Before birth the primordial alveoli appear as small bulges on the wall of respiratory bronchioles and terminal saccules. From 3rd to 8th the number of immature alveoli continues to increase. The major mechanism for increasing number of alveoli is the formation of connective tissue septa that subdivide existing primordial alveoli. About 50 million alveoli, one sixth of the adult number are present in the lungs of full term newborn infant. By about the eight year 300 million alveoli present in lungs Breathing movements occur before birth, exerting sufficient force to cause aspiration of some of amniotic fluid into lung. These movement are essential for normal development of lung. Fetal breathing movement, which increase as the time delivery approaches, probably condition the respiratory muscles. These movements stimulate lung development, possibly by creating a pressure gradient between lungs and amniotic fluid. Lung Expansion at Birth At birth about half the lungs are filled with fluid, derived from the amniotic cavity, lung and tracheal glands. Aeration of lungs at birth occur due rapid replacement of intra-alveolar fluid by air. The fluid in the lungs is cleared at birth by three routes: • Through mouth and nose by pressure on thorax during delivery • Into pulmonary capillaries • Into lymphatic and pulmonary Arteries and Veins Factors Important for normal Lung Development • Adequate thoracic space for lung growth • Fetal breathing movements • Adequate amniotic fluid volume Developmental Anomalies of Respiratory System • Esophageal Artesia • Trcheo-Esophageal Fistula • Congenital Diaphragmatic Hernia • Pulmonary Hypoplasia ESOPHAGEAL ATRESIA • Esophageal atresia is a congenital anomaly • Affects the alimentary tract • Esophagus ends in a blind-ended pouch rather than connecting normally to the stomach INCIDENCE • Occurs in approximately 1 in 4425 live births • May or may not occur with TEF • Isolated variant is rare ESOPHAGEAL ATRESIA PATHOPHYSIOLOGY • failure of the esophagus to develop as a continuous passage . • ends as a blind pouch. • failure of the recanalization of the esophagus during the eighth week of development ;no tracheoesophageal fistula • When associated with fistula there is deviation of tracheoesophageal septum posteriorly • Immediately diagnosed after birth • Should be promptly treated CONGENITAL TRACHEOESOPHAGEAL FISTULA • A fistula is an abnormal connection running either between two tubes or between a tube and a surface • TEF is an abnormal communication between trachea and oesophagus • arises due to failed fusion of the tracheoesophageal ridges during the third week of embryological development. • often found in association with other congenital anomalies • can be of diverse morphology and anatomical location, • Esophageal atresia results if the tracheoesophageal septum is deviated posteriorly. causes incomplete separation of the esophagus from the • laryngotracheal tube and results in tracheoesophageal fistula. TYPES OF TEF • Proximal esophageal atresia (esophagus continuous with the mouth ending in a blind loop superior to the sternal angle with a distal esophagus arising from the lower trachea or carina. • (Most common, up to 90% of cases--sometimes called a Type C fistula.) Proximal and distal esophageal bud--a normal esophagus • with a missing mid-segment. (Type A.) •Proximal esophageal termination on the lower trachea or carina with distal esophagus arising from the carina. (Type D.) If the two segments of esophagus communicate, this is termed an H-type fistula due to its resemblance to the letter H. •Proximal esophageal termination on the lower trachea with distal esophageal bud. (Type B.) TRACHEOESOPHAGEAL FISTULA • Maybe associated with other congenital • anomalies • called the VACTREL • (vertebral defect, anal • atresia, cardiac anomalies, • tracheoesophageal fistula, • renal anomalies, • esophageal atresia, limb • deformities) TRACHEO-ESOPHAGEAL FISTULA Different Types DIAGNOSIS ANDCLINICAL PRESENTATION • This condition is visible, after about 26 weeks, on an ultrasound, may be detected soon after birth in a newborn by copious salivation • choking, • Coughing • cyanosis • Gastric distention • All symptoms coincident with the onset of feeding . COMPLICATION Aspiration pneumonia when attempt to feed the milk collects in the blind pouch and overflows into the trachea and lungs. Gastric acid aspiration as fistula between the lower esophagus and trachea may allow stomach acid to flow into the lungs and cause damage . TREATMENT • vary depending on its severity • The most immediate and effective treatment in the majority of cases is a surgical repair to close the fistula/s and reconnect the two ends of the esophagus to each other • .When gap is too large, a gastrostomy is performed, allowing tube feedings into the stomach through the abdominal wall. • Followed by repairing of oesophagus by interposing a segment of gut between the upper and lower segments months or years later, HYALINE MEMBRANE DISEASE Respiratory Distress Syndrome RDS Seen among premature infants Insufficient surfactant resulting in high membrane tension thus collapse of alveoli Many hyaline membrane and lamellar bodies present in collapsed alveoli Incidence - RDS occurs primarily in the immature lung. (1) 60 % of cases occur in infants born at less than 28 weeks’ gestation (2) 5 % of cases occur in infants born at less than 37 weeks’ gestation HYALINE MEMBRANE DISEASE Respiratory Distress Syndrome CLINICAL FINDINGS • Onset Usually less than 2-5 hours after birth • Increases in severity from 24 to 48 hours • gradual improvement after 48-72 hours • Abnormal retraction of chest wall • Cyanosis • Expiratory grunting • Increased respiratory rate PULMONARY HYPOPLASIA Pulmonary hypoplasia results when lungs are compressed by abnormally positioned abdominal viscera and cannot develop normally or expand at birth .It is commonly caused by congenital posterolateral diaphragmatic hernia . CONGENITAL DIAPHRAGMATIC HERNIA • Failure of the pleuroperitoneal foramen (foramen of Bochdalek) to close allows viscera into thorax. Intestine, stomach or spleen can enter the pleural cavity, compressing the lung.