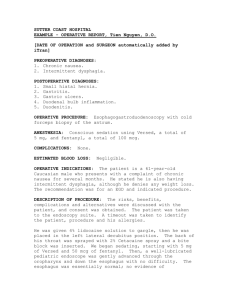
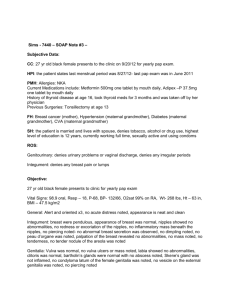
POSTOPERATIVE DIAGNOSIS: Reflux
advertisement

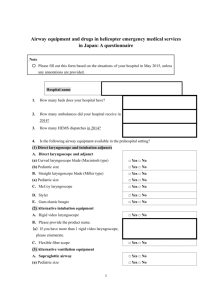
POSTOPERATIVE DIAGNOSIS: ANESTHESIA: Reflux. General. ESTIMATED BLOOD LOSS: None. INDICATIONS FOR SURGERY: This is a 31-year-old female referred to me for recurrent hoarseness for several months, who had been on some medication. Risks and benefits and alternatives to surgery, general anesthesia, laryngospasm, and no guarantee of final outcome including the need for further medical or surgical intervention, including any unanticipated surgical complications were fully explained to the patient. She fully understood and consented to the procedure. PROCEDURE IN DETAIL: Patient was identified and taken to the OR suite, where she was administered a general anesthetic. The mouth was then manually palpated and no masses were noted. The anterior commissure laryngoscope was slowly introduced into the mouth and advanced to the base of the tongue. No masses were noted at the base of the tongue or vallecula. Then the laryngoscope was further advanced down to the hypopharynx and directed to the right and left piriform sinuses, and again, no masses were noted. The laryngoscope was used to lift the epiglottis anteriorly and was advanced further down to the hypopharynx. At this time, the true and false vocal cords and postcricoid area were fully visualized, which at the time, the laryngoscope was adapted to be loose and was suspended on a Mayo stand. The microscope was then brought to the field and no masses were noted. Both arytenoids were noted to moderately inflamed. The laryngoscope was then removed from the mouth. The patient tolerated the procedure without incident. She was transferred to the PACU stable in satisfactory condition. She was sent home on Robitussin-DM for postoperative pain. She was also given appointment one week from now.