EGD Operative Report: Nausea, Dysphagia, Gastritis
advertisement
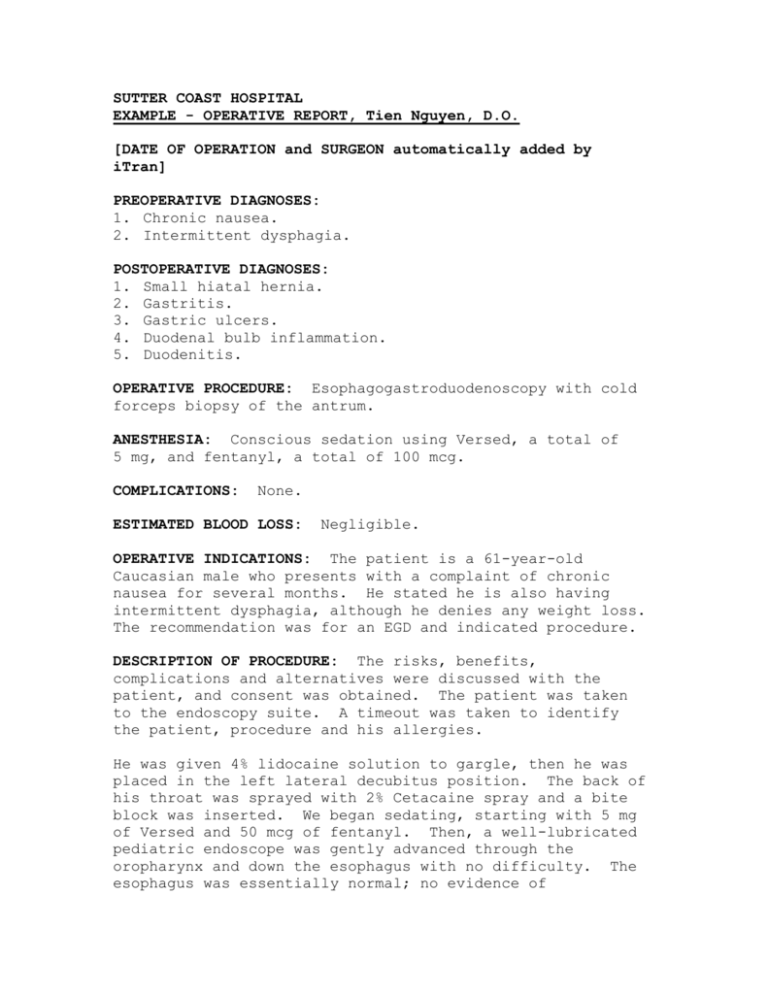
SUTTER COAST HOSPITAL EXAMPLE - OPERATIVE REPORT, Tien Nguyen, D.O. [DATE OF OPERATION and SURGEON automatically added by iTran] PREOPERATIVE DIAGNOSES: 1. Chronic nausea. 2. Intermittent dysphagia. POSTOPERATIVE DIAGNOSES: 1. Small hiatal hernia. 2. Gastritis. 3. Gastric ulcers. 4. Duodenal bulb inflammation. 5. Duodenitis. OPERATIVE PROCEDURE: Esophagogastroduodenoscopy with cold forceps biopsy of the antrum. ANESTHESIA: Conscious sedation using Versed, a total of 5 mg, and fentanyl, a total of 100 mcg. COMPLICATIONS: None. ESTIMATED BLOOD LOSS: Negligible. OPERATIVE INDICATIONS: The patient is a 61-year-old Caucasian male who presents with a complaint of chronic nausea for several months. He stated he is also having intermittent dysphagia, although he denies any weight loss. The recommendation was for an EGD and indicated procedure. DESCRIPTION OF PROCEDURE: The risks, benefits, complications and alternatives were discussed with the patient, and consent was obtained. The patient was taken to the endoscopy suite. A timeout was taken to identify the patient, procedure and his allergies. He was given 4% lidocaine solution to gargle, then he was placed in the left lateral decubitus position. The back of his throat was sprayed with 2% Cetacaine spray and a bite block was inserted. We began sedating, starting with 5 mg of Versed and 50 mcg of fentanyl. Then, a well-lubricated pediatric endoscope was gently advanced through the oropharynx and down the esophagus with no difficulty. The esophagus was essentially normal; no evidence of strictures, no varices and no bleeding. A minimal amount of dysplastic changes were noted at the GE junction. Inside the stomach, the scope was retroflexed and a small hiatal hernia was noted. There was diffuse gastritis noted, mainly in the antrum and prepyloric area. The scope was advanced into the pylorus. There was inflammation noted in the duodenal bulb. We also noted inflammation without any active bleeding inside of the first portion of the duodenum. The scope was pulled back into the prepyloric area, whereby a cold forceps biopsy was taken for SRU. Another cold forceps biopsy was taken in the antrum near one of the gastric ulcers. Then, I evacuated the stomach of as much of the air and fluid as possible. I removed the scope and the bite block completely. The patient tolerated the procedure well and was taken to the Recovery Room in satisfactory condition. RECOMMENDATIONS: I recommend that the patient be placed on Nexium daily for another 2 months, and for the patient to begin on a low-acidic diet. Also, I recommend the patient stop smoking.