Robert Romano
advertisement

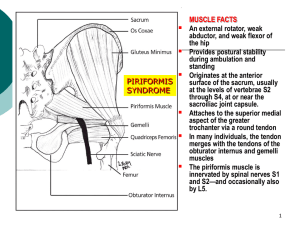
Dr. Robert T. Romano, D.C. - Magnetic Resonance Imaging of the Sacral Plexus and Piriformis Muscles This article describes an experiment whereby researches examined the relationship between the piriformis muscle and the sacral nerve roots. Chiropractors are aware that the piriformis, when dysfunctional, can cause symptoms similar to “sciatica” due to the variability of the nerve roots relationship to the piriformis muscle. Many chiropractic textbooks say that the sciatic nerve can pass above, through, or below the piriformis muscle, causing various symptoms of nerve impingement due to contraction of the piriformis. Piriformis syndrome is a “controversial” diagnosis usually applied to patients with complaints of sciatic pain in the buttocks and the thigh, exacerbated by prolonged sitting or walking, and typically without sensory deficit, and which cannot be distinguished to be from a disc or other issue. This study involved 100 patients who were to undergo routine MRI examination. While doing their prescribed MRI, the researchers also took axial and sagittal T1-weighted MRI of the sacrum to visualize the piriformis and the sacral nerve roots. Each patient was examined bilaterally (two sets of nerve roots and 2 piriformis muscles), totaling 200 samples to study. The study also aimed to correlate symptoms indicative of piriformis syndrome with radiological findings. Unfortunately (for us!), none of the 100 patients had symptoms suggestive of “classic” piriformis syndrome, so that correlation was not able to be done adequately. This study was primarily undertaken to elucidate the anatomical variations of the piriformis and its relationship to the sacral plexus roots, with the goal of perhaps shedding some light on the poorly understood condition called “piriformis syndrome”. The results showed that there is variability in the manner with which the sacral roots relate to the piriformis, and there is also variability of the size of the piriformis muscle when compared bilaterally in the same individual. Specifically, the S1 nerve roots pass above the piriformis more than 99% of the time, the S3 roots pass through the piriformis muscle 97% of the time, and the S2 goes through 75% of the time (other 25% went above). S4 was almost always below the muscle. It is interesting that S2 is less likely than S3 to pass through the muscle. Also clinically important is the variation in piriformis size, with asymmetry common. About 20% of the patients had piriformis asymmetry greater than 3mm, with differences as big as 8mm between piriformis muscle sizes. None of the patients with asymmetry had piriformis syndrome. The researchers concluded that the S2 nerve root passing through the piriformis is a normal variation, and is not associated with the symptoms of piriformis syndrome in the patients involved in the study. A limitation of the study was the fact that the symptoms of piriformis syndrome were not arrived at via examination, but instead with a questionnaire, and actually physically examining a patient is a more sensitive way to test for piriformis syndrome.