Document
advertisement

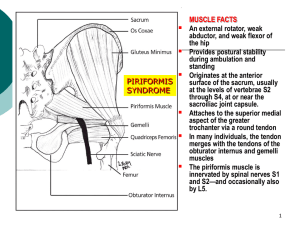
Piriformis Syndrome • Situation where the piriformis muscle is compressing the sciatic nerve resulting in sciatic neuropathy Piriformis Syndrome • The PM and sciatic nerve both exit the pelvis through the greater sciatic notch Anatomic Characteristics • The piriformis muscle acts as an external rotator, weak abductor, and weak flexor of the hip, providing postural stability during ambulation and standing. • The piriformis muscle originates at the anterior surface of the sacrum, usually at the levels of vertebrae S2 through S4, at or near the sacroiliac joint capsule. The muscle attaches to the superior medial aspect of the greater trochanter via a round tendon that, in many individuals, is merged with the tendons of the obturator internus and gemelli muscles (Figure 1).1,13,14 • The piriformis muscle is innervated by spinal nerves S1 and S2—and occasionallyalso by L5. History • Yeoman first describe this relationship in 1928 • Robinson first coined the term piriformis syndrome in 1947 Anatomical Variations • Numerous anatomical variations of this relationship Causes • Intrinsic injury – to the muscle itself • Extrinsic injury – compression at the pelvic outlet Causes • A combination of weaker abductors and relatively stronger adductors can also cause piriformis syndrome. • Problems related to sacroiliac joints such as stiffness, overstress etc. can also lead to this condition as the stress/stiffness is taken care by surrounding gluteal and piriformis muscles. • A rotational movement of foot occurs at the subtalar and talocalcaneonavicular joints, which is known as pronation. If this movement is overdone, it can cause the knee to turn medially more than the natural degree of rotation, this is prevented with the help of piriformis muscles. As the piriformis muscles are not made to bear such a high stress/pressure, it can lead to development of piriformis syndrome. Causes • Overstress and strain on the sciatic nerve by piriformis muscle is the main cause of this syndrome. • Trauma, any type of injury or stress in the area surrounding piriformis muscles or disorders related to nerves and muscles, which cause overstress/strain on the piriformis muscles can lead to development of this syndrome. • Inactivation of gluteal muscles that play an important role in helping and supporting hip extension and piriformis muscles in external rotation of the femur caused by overstressed and overactive hip flexors; is also considered to lead to onset of this syndrome. • People involved in exercise, sports (race, cycling etc.) and activities that need to use forward postures/movements of body are prone to develop piriformis syndrome as a result of the stress and strain on the piriformis muscles. In order to compensate the stress and strain caused by the forward movement, one should use stretching and some other exercises so that piriformis muscles can be relaxed and strengthened. Controversial Diagnosis • No consensus among clinicians on the validity of this entity and no documentation of its incidence Epidemiologic Considerations • Piriformis syndrome occurs most frequently during the fourth and fifth decades of life and affects individuals of all occupations and activity levels. • Reported incidence rates for piriformis syndrome among patients with low back pain vary widely, from 5% to 36%. • Piriformis syndrome is more common in women than men, possibly because of biomechanics associated with the wider quadriceps femoris muscle angle (ie, “Q angle”) in the os coxae (pelvis) of women Symptoms • Buttock pain with or without pain into the buttock • Chronic and acute cases • Often a hx of minor trauma such as falling on the buttock Symptoms Symptoms • Sitting on a hard surfaces will exacerbate the symptoms of pain and occasional numbness and paresthesias without weakness Activites • that produce the motion of hip adduction and internal rotation such as cross country skiing and the over head serve in tennis may also exacerbate the symptoms Symptoms • Because of the relationship of the piriformis and the lateral pelvic wall, patients may experience pain with bowel movements and women may complain of dyspareunia Functional limitations • Pain with prolong sitting on hard surfaces such as in church pews, • Pain with activities that produce hip IR and adduction What is wallet sign? Is your wallet hurting you? wallet neuritis What is Pace sign? Physical exam – Pace Sign • Contraction of the piriformis muscle with resistant to active hip external rotation and abduction may reproduce pain or asymmetrical weakness Pace Sign (FAIR Test) • FAIR (flexion, adduction, and internal rotation) test involves the recurrence of sciatic symptoms. • The FAIR test is performed with the patient in a lateral recumbent position, with the affected side up, the hip flexed to an angle of 60 degrees, and the knee flexed to an angle of 60 degrees to 90 degrees. While stabilizing the hip, the examiner internally rotates and adducts the hip by applying downward pressure to the knee. FAIR Test • Fishman found the FAIR test to have sensitivity and specificity of 0.881 and 0.832, respectively. • Alternatively, the FAIR test can be performed with the patient supine or seated, knee and hip flexed, and hip medially rotated, while the patient resists examiner attempts to externally rotate and abduct the hip. • The FAIR test result is positive if sciatic symptoms are recreated. FAIR Test • FAIR (flexion, adduction, and internal rotation) test. • performed with the patient in a lateral recumbent position, with • the affected side up, the hip flexed to an angle of 60 degrees, and • the knee flexed to an angle of 60 degrees to 90 degrees. While stabilizing • the hip, the examiner internally rotates and adducts the hip • by applying downward pressure to the knee. What is a positive piriformis sign? Positive Piriformis Sign • Contracted piriformis muscle also causes ipsilateral external hip rotation. • When a patient with piriformis syndrome is relaxed in the supine position, the ipsilateral foot is externally rotated (a feature referred to as a positive piriformis sign. • Active efforts to bring the foot to midline result in pain. What is a positive Frieberg sign? Physical exam • Positive Freiberg test – passive hip abduction and internal rotation may compress the sciatic nerve reproducing the pain What is Beatty maneuver? Beatty Maneuver • Patient lies on the uninvolved side and abducts the involved thigh upward, which elicits pain. • If sciatic symptoms are recreated, the test result is positive. What muscle is functionally related to the SI joint ? Short leg and Sacrum Torsion • In most cases of piriformis syndrome, the sacrum is anteriorly rotated toward the ipsilateral side on a contralateral oblique axis, resulting in compensatory rotation of the lower lumbar vertebrae in the opposite direction. • For example, piriformis syndrome on the right side would cause a left-on-left forward sacral torsion with L5 rotated right. Sacral rotation often creates ipsilateral physiologic short leg. Physical exam • Normal neuro exam (strength and reflexes) • Tenderness to palpation is experience from the sacrum to the greater trochanteric representing an area of the Piriformis Muscle • Palpable taut band on rectal exam Differential Diagnosis Secondary causes: – Superior and inferior gluteal artery aneurysm – Benign pelvic tumor – Endometiosis – Myositis ossificans Dx that mimic PM Lumbar facet syndrome L5S1 radiculopathy Diagnostic testing • • • • Clinical diagnosis MRI and CT rule out other disorders Prolong H wave EMG to r/o other things Treatment • Throughout the physical evaluation of patients, clinicians should maintain a high index of suspicion for piriformis syndrome. • Early conservative treatment is the most effective treatment,as noted by Fishman who reported that more than 79% of patients with piriformis syndrome had symptom reduction with use of nonsteroidal anti-inflammatory drugs(NSAIDs), muscle relaxants, ice, and rest. Treatment • NSAID • Heat • cushions Treatment • Stretching of the piriformis muscle and strengthening of the abductor and adductor muscles should also be included inpatient treatment plans. • A manual medicine approach may combine muscle stretches, spray and stretch technique, and soft tissue, myofascial, muscle energy, and thrust techniques to address all somatic dysfunctions in the patient with piriformis syndrome. • Treatment • In particular, the strengthening of the adductor muscles of the hip has been shown to be beneficial for patients with piriformis syndrome. • Several studies have reported that additional benefit can be derived from physical therapy modalities, such as heat therapy, cold therapy, BTX-A injection, and ultrasound. • Heat or cold therapy is usually most effectively applied before the physical therapy or home therapy sessions because it may lessen the discomfort associated with direct treatment applied to an irritated or tense piriformis muscle. • Injections of BTX-A, when used as an adjunct to physical therapy, have been shown to produce more pain relief than lidocaine with steroids Counterstrain Technique • Three tender point locations can be addressed with counterstrain—at the midpole sacrum, piriformis muscle, and posteromedial trochanter. • To position a patient for counterstrain treatment, the patient is generally asked to lie in a prone positionwith the affected side of the body at the edge of the examination table. • • In performing the counterstrain technique, the physician brings the patient’s affected leg overthe side of the table, placing it into flexion at the hip and knee, with abduction and external rotation at the hip . Physical Therapy • Patients with piriformis syndrome may be treated with physical therapy involving a variety of motion exercises and stretching techniques. • It is important for the physician to clearly demonstrate the stretches that the patient is expected to perform. • It is also advisable to have the patient perform these exercises for the first time in the office, where the physician can observe and modify the patient’s techniques, as needed. • If the patient demonstrates excessive difficulty in understanding or performing the exercises, the physician can refer the patient to a licensed physical therapist for assistance. • If a patient is able to perform the required exercises at home, he or she should be advised to do so in multiple short sessions each day, with each session lasting only a few minutes. Stretching Strengthening • Gluteus medius – theraband around the ankles and walking sideways Correct Biomechanic abnormalities • • • • • • Increase pronation Hip abductor weakness Lower lumbar dysfunction SI hypo mobility Hamstring tightness Lead to a gait with hip in ER, shortened leg length and a functional short leg Ultrasound and stretch • Hip IR above 90 degrees of hip flexion • Hip ER below 90 degrees of hip flexion Other treatment options • Injection 1cm caudal and 2cm lateral to the lower border of the SI joint • Caudal epidural • Surgical release Physiatric Prescription