Lecture: Circulatory Physiology
advertisement

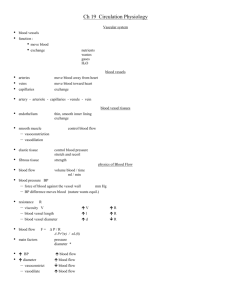
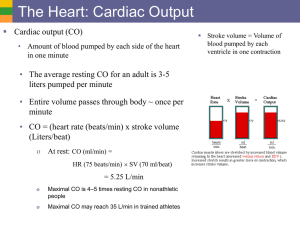
Lecture: Circulatory Physiology I. Factors Involved in Blood Circulation A. Blood Flow - the actual VOLUME of blood moving through a particular site (vessel or organ) over a certain TIME period (liter/hour, ml/min) B. Blood Pressure - the FORCE exerted on the wall of a blood vessel by the blood contained within (millimeters of Mercury; mm Hg) blood pressure = the systemic arterial pressure of large vessels of the body (mm Hg) C. Resistance to Flow (Peripheral Resistance) - the FORCE resisting the flow of blood through a vessel (usually from friction) 1. viscosity - a measure of the "thickness" or "stickiness" of a fluid flowing through a pipe a. b. D. V water < V blood < V toothpaste water flows easier than blood 2. tube length - the longer the vessel, the greater the drop in pressure due to friction 3. tube diameter - smaller diameter = greater friction Relation Between Blood Flow, Pressure, Resistance difference in blood pressure ( P) Blood Flow (F) = peripheral resistance (R) a. b. c. d. II. increased P -> increased flow decreased P -> decreased flow increased R (vasoconstriction) -> DECREASED flow decreased R (vasodilation) -> INCREASED flow Systemic Blood Pressure A. Blood Pressure Near the Heart 1. 2. HEART produces blood pressure by pumping the blood Blood pressure decreases with distance from Heart 3. systolic arterial blood pressure - pressure in aorta (& major arteries) in middle of ventricular contraction (120 mm Hg in healthy adult) 4. diastolic arterial blood pressure - pressure in aorta (& major arteries) during ventricular diastole, when semilunar valves are closed (80 mm Hg in healthy adult) 5. mean arterial pressure (MAP) - the "average" blood pressure produced by the heart (93 mm Hg in healthy adult) mean arterial pressure = diastolic pressure + 1/3 pulse pressure ** 6. pulse pressure = systolic pressure - diastolic pressure blood pressure decreases throughout system L ventricle arteries arterioles capillaries venous R atrium 7. -->120 mm Hg -->120 - 60 mm Hg -->60 - 40 mm Hg -->40 - 20 mm Hg -->20 - 10 mm Hg -->10 - 0 mm Hg venous return - venous blood pressure is so low, other factors contribute to venous blood flow a. respiratory pump - breathing action of thorax "squeezes" blood back toward the heart b. muscular pump - contraction/relaxation of skeletal muscles "milk" blood up veins to heart III. Factors Affecting Blood Pressure A. Cardiac Output ( = stroke volume X heart rate) CO 1. 2. 3. B. = 70 ml/beat x 60 beats/min = 4200 ml/min increased cardiac output -> increased blood pressure increased stroke volume -> increased blood pressure increased heart rate -> increased blood pressure arteriole constriction ---> increased blood pressure resistance inversely proportional to the "fourth power" of the radius change Blood Volume 1. 2. 3. 4. IV. SV (ml/beat) x HR (beats/min) Peripheral Resistance 1. 2. C. = hemorrhage - decrease in blood pressure salt/fluid - increase in blood pressure polycythemia - increase in blood viscosity RBC anemia - decrease in blood viscosity Regulation of Blood Pressure A. Nervous System Control 1. control of arteriole diameter 2. 3. directs blood flow to proper organs and tissues that need it REFLEX PATHWAY: baroreceptors/chemoreceptors/brain afferent nerve fibers medulla (vasomotor center) vasomotor (efferent) nerve fibers smooth muscle of arterioles B. Vasomotor Fibers to Smooth Muscle of Arterioles 1. C. sympathetic fibers that release norepinephrine (NE); cause vasoconstriction of arterioles Vasomotor Center of the Medulla 1. 2. 3. D. sympathetic neuron cell bodies in the medulla receive input from baroreceptors, chemoreceptors, and brain vasomotor tone - general constricted state of arterioles set by vasomotor center Baroreceptors 1. 2. blood pressure receptors large arteries (carotid sinuses, aortic arch, neck/thorax arteries) send blood pressure information to vasomotor center of medulla increased pressure inhibits vasomotor center vasodilation E. F. --> --> decreased pressure --> stimulates vasomotor center -> vasoconstriction Chemoreceptors 1. located in aortic arch and carotid arteries a. carotid and aortic bodies 2. monitor OXYGEN and pH levels of the blood low OXYGEN or low pH -------> increase blood pressure, return blood to lungs quickly Higher Brain Centers Control on BP 1. G. --> --> --> --> hypothalamus & cortex also effect vasomotor area Chemical Controls of Blood Pressure 1. hormones of adrenal medulla - "fight-or-flight" response to fear; release of norepinephrine and epinephrine from adrenal medulla; causes vasoconstriction and increased BP 2. atrial natriuretic factor (ANF) - secreted by the atria of the heart, promotes general decline in blood pressure kidney releasing more Na+ and water, reducing fluid volume 3. antidiuretic hormone (ADH) - released by the hypothalamus, causes increase in blood pressure by getting the kidneys to conserve water in the body; e.g. during hypotensive situations 4. endothelium derived factors a. b. 5. H. endothelin - strong vasoconstrictor endothelium derived relaxing factor - vasodilation alcohol - causes vasodilation Renal (Kidney) Regulation 1. direct regulation - fluid loss through urine a. b. 2. low pressure/volume --> conserve water high pressure/volume --> release more water renin-angiotensin mechanism low blood pressure --> release of renin --> formation of angiotensin II--> vasoconstriction release of aldosterone --> Na+/water reabsorption (by kidney) V. Variations in Blood Pressure A. Measuring Blood Pressure 1. vital signs - blood pressure, pulse, respiratory rate, and body temperature 2. auscultory method of blood pressure measurement a. b. c. d. B. “sphygmomanometer” wrapped around upper arm inflate above systolic pressure of brachial a. pressure released, first sounds - systolic pr. disappearance of sounds - diastolic pr. Hypotension (below normal blood pressure, < 100/60) 1. factors - age, physical conditioning, illness 2. orthostatic hypotension - generally in elderly, drop in blood pressure during postural changes 3. chronic hypotension - ongoing low blood pressure a. b. c. d. low blood protein levels (nutrition) Addison’s disease (adrenal cortex malfunction) hypothyroidism also sign of various types of cancer C. Hypertension (above normal blood pressure at rest, > 140/90) 1. 2. factors - weight, exercise, emotions, stress chronic hypertension - ongoing high blood pressure a. b. c. d. prevalent in obese and elderly leads to heart disease, renal failure, stroke also leads to more arteriosclerosis primary hypertension - unidentified source i. ii. iii. iv. e. secondary hypertension - identifiable disorder i. ii. iii. VI. high Na+, cholesterol, fat levels clear genetic component (in families) diuretics - promote water removal NE blockers - slow vasoconstriction kidney disorders endocrine (hormone) disorders arteriosclerosis Blood Flow in the Body A. General Features 1. 2. 3. 4. 5. B. delivery of oxygen and removal of carbon dioxide gas exchange in the lungs absorption and delivery of nutrients from GI tract processing/waste removal in the kidneys normal blood flow at rest abdominal organs 24% skeletal muscle 20% kidneys 20% brain 13% heart 4% other 15% Velocity of Blood Flow 1. velocity directly related to the TOTAL cross-sectional area of the vessel(s) FASTEST SLOWEST C. aorta arteries arterioles capillaries 40-50 cm/s 20-40 cm/s 1-20 cm/s 0.1-1 cm/s Local Regulation of Blood Flow 1. autoregulation - regulation of blood flow by altering arteriole diameter a. b. c. D. 2. myogenic response - change in flow through arteriole in response to stretch of smooth muscle 3. reactive hyperemia - increase in blood flow to area where an occlusion has occurred 4. increased vasculature - results from prolonged lack of oxygen/nutrients to an area (eg. heart) Blood Flow to Skeletal Muscles 1. active (exercise) hyperemia - increased blood flow to muscles during heavy activity a. b. E. decreased oxygen and increased lactic acid visceral organ blood flow is decreased Blood Flow to The Brain 1. 2. 3. F. oxygen and carbon dioxide levels prostaglandins, histamines, kinins needy areas --> more blood flow MUST maintain constant blood flow (750 ml/min) sensitive to low pH and high carbon dioxide blood pressure tightly regulated in the brain a. fainting -> below 60 mm Hg b. edema (brain swelling) -> above 180 mm Hg Blood Flow to The Skin 1. intimately involved in temperature regulation increased body temperature -> hypothalamic inhibition of vasomotor area -> vasodilation of vessels in skin -> increased blood flow -> sweating -> (bradykinin -> more vasodilation) G. Blood Flow to the Lungs 1. 2. H. Blood Flow to the Heart 1. 2. VII. short pathway from heart, less pressure required low oxygen level --> vasoconstriction blood to coronary arteries during diastole vasodilation from ADP and carbon dioxide Blood Flow in the Capillaries A. B. C. Exchange of Gases and Nutrients 1. diffusion - all molecules move DOWN the concentration gradient (from HIGH to LOW) into or out of the blood 2. oxygen/nutrients carbon dioxide/ wastes (blood (body cells ------> body cells) ------> blood) Fluid Movements 1. hydrostatic pressure - force from the capillary wall on the blood itself a. filtration pressure - the pressure forcing fluid and solutes through capillary clefts 2. 3. osmotic pressure - force driving fluid in the direction of HIGHER solute concentration movement out: Hydrostatic pressure > Osmotic difference movement in : Hydrostatic pressure < Osmotic difference 4. normal fluid movement 1.5 ml/min in the entire body Circulatory Shock 1. circulatory shock - blood pressure gets so low that blood will not flow adequately 2. hypovolemic shock - circulatory shock resulting from loss of fluid (bleeding, diarrhea, burn) a. heart rate increases rapidly b. general vasoconstriction of vessels 3. vascular shock - extreme vasodilation causes sudden drop in blood pressure a. snake and spider bites with NE blockers b. septicemia - bacterial infection 4. cardiogenic shock - heart is unable to provide sufficient blood pressure