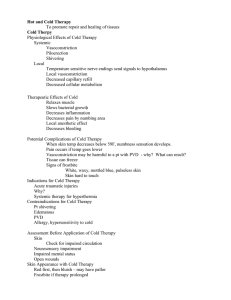
Heat and Cold Application
advertisement

Principles for Nursing Practice Heat and Cold Application Dr. Belal Hijji, RN, PhD February 25, 2012 Learning Outcomes At the end of this lecture, students will be able to: • Discuss the therapeutic uses of heat and cold therapy and their methods of application. 2 Regulation of Heat and Cold • The hypothalamus acts as a thermostat to regulate body temperature. When the body temperature is either too high or too low, the hypothalamus responds by instituting temperaturedecreasing (vasodilation, sweating) or temperature-increasing (vasoconstriction, shivering) mechanisms to restore normal body temperature. • Local responses to heat and cold occur through stimulation of temperature-sensitive receptors in the skin. Impulses travel from the periphery to the hypothalamus and the cerebral cortex. The hypothalamus then initiates heat-producing or heat-reducing reactions of the body. The conscious sensations of temperature are aroused in the cerebral cortex. 3 Heat Application and Its Benefits • Heat is a nursing measure used to reduce pain and promote healing. After application, it causes maximum vasodilation in 20 to 30 minutes and increases blood flow to the affected area. After this period, reflex vasoconstriction occurs along with tissue congestion. Periodic removal and reapplication of heat will restore vasodilation. • Heat increases delivery of oxygen, nutrients, leukocytes, and antibodies to ease the inflammatory process. It facilitates removal of wastes and toxins, and produces a local warming effect. In addition, heat increases absorption of fluid by capillaries and promotes removal of excess fluid from interstitial spaces, thereby reducing edema. Finally, heat promotes muscle relaxation and decreases pain from spasm or stiffness. 4 Cold Application and Its Benefits • Cold application lowers the skin and underlying tissues temperature and causes vasoconstriction, which reduces blood flow to the affected area and produces skin pallor, numbness, and pain. Maximum vasoconstriction occurs at 15°C. At temperatures below 15°C, the vessels begin to dilate. Prolonged exposure to cold results in a reflex vasodilation. • Vasodilation and vasoconstriction of the blood vessels in the skin result primarily from increased sensitivity of the vessels to nerve stimulation and from a protective reflex response that passes to the spinal cord and then back to the vessels. 5 Cold Application and Its Benefits (Continued…) • The benefits of cold application include decreasing blood flow to site of injury, thereby decreasing inflammation and edema formation, and facilitating clotting and control of bleeding. • In addition, cold reduces tissues’ oxygen consumption, and raises the threshold of pain receptors, thereby decreasing pain. 6 Factors Affecting Heat and Cold Tolerance • Body part: Certain areas of the skin have a sensitivity to temperature variations. The inner aspect of the wrist and forearm are temperature-sensitive, while the back of the hand and the foot are not as sensitive. • Duration of application: Therapeutic benefits of heat and cold applications are achieved with short periods of exposure to temperature variations. Tolerance increases as the length of exposure increases. • Damage to body surface area: Injured skin areas are more sensitive than intact areas to temperature variations. 7 Factors Affecting Heat and Cold Tolerance (Continued..) • Physical condition: Neurosensory impairments may interfere with the reception and perception of stimuli. Diabetes mellitus and atherosclerosis can impair neurosensory pathways and result in deficits in sensation, thus, increasing the risk of injury. • Age: Thinner skin layers in children and elderly people increase the risk for burns from heat and cold applications. Older adults have a decreased sensitivity to pain. 8 Nursing Checklist for Heat and Cold Application • Obtain a physician’s order that details the site to be treated, the type of therapy, and the frequency and duration of application. • Select temperature on the basis of client status and agency policy. • Thoroughly explain procedure and expected benefits to client. • Assess client’s status before, during, and after treatment is performed to prevent injury. • Document effects of therapy. 9 Thank You Any Questions?