BIOLOGY 206 CHAPTER 20: BLOOD VESSELS
advertisement

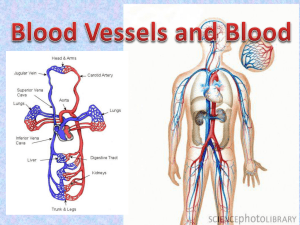
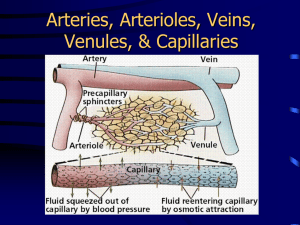
BIOLOGY 206 CHAPTER 19: BLOOD VESSELS: LAUREL; SPRING 2007 I. General features of blood vessel structure A. Overview 1. 5 major types of blood vessels are a. Arteries and arterioles which carry blood away from heart. ** b. Capillaries join arterioles and venules and are sites where diffusion, filtration and osmosis occur, hence they are the functional units of the circulatory system c. Venules and veins which carry blood back from tissues to heart. 2. Generalized blood flow: heart --> artery --> arteriole --> capillary --> venule --> vein --> heart B. Structure of blood vessel walls. 1. All vessels except capillaries have 3 distinct layers, tunics, surrounding a central tubular opening, the lumen. 2. Tunica intima = innermost layer that lines the lumen. a. It contains the endothelium which is made of simple squamous epithelium which is smooth to decrease friction with blood. b. Found in all blood vessels, and is the only layer in capillaries. 3. Tunica media = middle layer of smooth muscle and elastic connective tissue * a. Contraction controlled by vasomotor fibers of sympathetic division of ANS such that an increase in sympathetic stimulation causes vasoconstriction (lumen gets smaller) and a decrease in sympathetic stimulation causes vasodilation (lumen gets larger) b. Small changes in lumen diameter greatly influence blood flow (constriction restricts blood flow to that area and redirects blood elsewhere). * c. Small changes in lumen diameter (especially of arterioles) greatly influence blood pressure. Vasoconstriction increases blood pressure and vasodilation decreases blood pressure in the artery preceding arteriole. d. Bulkiest of the 3 layers and most evident in arteries. 4. Tunica adventitia = outermost layer composed of collagen fibers to protect the vessels and anchor them to surrounding structures. a. Contains nerve fibers and lymphatic vessels. b. Most abundant layer in veins. II. Types of Arteries (all carry blood away from heart) A. Elastic arteries (conducting arteries) 1. Largest, most elastic, thick walled, and close to heart a. Aorta 1 III. b. Pulmonary trunk 2. Not significant in vasoconstriction, but serve as low resistance conduit from heart to medium sized arteries. 3. Exhibit 2 important properties: a. Elasticity which allows them to expand under pressure. b. Contractility which allows them to recoil and keep blood flowing continuously B. Muscular arteries (distributing arteries) 1. Medium-sized arteries which carry blood from elastic arteries to specific organs. 2. Have proportionally more smooth muscle and less elastic tissue. 3. They are more active in vasoconstriction but are less distensible than elastic arteries. C. Arterioles 1. Smallest of arterial vessels with lots of smooth muscle. (30 um in diameter) 2. Feed directly into capillary beds. * 3. Most important vessels to control blood pressure and flow into capillary beds. a. Vasoconstriction --> bypass bed b. Vasodilation --> flow into bed. D. Arterial pulse 1. = alternating expansion and recoil of arteries during each cardiac cycle. 2. Easy way to count heart rate. 3. Lying down = 60, sitting = 70, stand quickly = 80 Capillaries A. General Features 1. 8-10 um in diameter, just large enough for a single RBC to slip through. 2. Form beds of 10 to 100 capillaries with large cross-sectional area. 3. Generally 1 mm long B. Structure and function 1. Only vessel to have only tunica intima. 2. Role is exchange of materials through osmosis, diffusion, diapedesis, etc. C. Types of capillaries 1. Continuous capillaries a. Most common, especially in skin and muscles b. Have uninterrupted endothelial lining; cells joined laterally by tight junctions which are incomplete such that there are gaps (intercellular clefts) in them to allow passage of fluids and small solutes to pass into interstitial fluid. 2. Fenestrated capillaries 2 a. IV. Similar to continuous but their plasma membranes are full of pores (fenestrations) b. Have increased permeability c. Small intestines and endocrine glands, glomeruli of kidneys 3. Sinusoids a. Highly modified and very leaky to allow large molecules such as proteins and blood cells to pass through them. b. Fenestrated and have larger intercellular clefts such that proteins can pass c. liver, bone marrow, and lymphoid tissue D. Capillary Beds 1. Capillaries form beds of 10 - 100 capillaries with large X-sectional area . 2. Flow in the beds is controlled by precapillary sphincters at junction between arteriole and capillary. 3. When sphincters are open blood flows into all capillaries in the bed and exchange occurs 4. When the sphincters are closed blood only flows into a thoroughfare channel such that exchange is bypassed. Veins (return blood to the heart) A. Venules 1. Formed when capillaries unite. 2. The smallest are almost entirely endothelium. B. Veins 1. All 3 tunics a. Adventitia most abundant. b. Relatively little smooth muscle in tunica media when compared to arteries. 2. Walls thinner and lumens larger than those of corresponding arteries . 3. Thinness allows them to accommodate large volumesof blood. a. Up to 65% of blood volume usually found in veins. * b. So act as blood reservoirs. 4. Can be thin because blood pressure is very low in them. 5. One-way Valves are needed, however, to keep bloodfrom flowing backward and down with gravity. Most abundant in limbs. 6. heart. a. Are folds in the endothelium (tunica intima) Other adaptations to help return blood to the a. Large lumens = low resistance. 3 b. c. Respiratory pump =inhalation produces increased pressure in abdomen which squeezes veins and pushes blood up, and decreased pressure in thoracic cavity which pulls blood up. Skeletal muscle pump= contractions "milk" blood toward heart. 7. Varicose veins are dilated areas in veins because of damaged valves. Superficial veins most susceptible because they receive least structural/muscular support. a. Causes: obesity, pregnancy, prolonged standing in one position, heredity, straining. 8. Anastomoses: interconnecting vascular channels a. Much more common in veins than in arteries 9. Hemorrhoids = varicosity in anal canal. V. Introduction to Blood flow, blood pressure, and resistance A. Definition of terms 1. Blood flow (F) is the volume of blood passing through a particular vessel at a particular time (ml/min) a. Blood flow through an individual organ may vary widely depending on immediate needs 2. Blood pressure (BP) is the force/unit area exerted on the wall of a blood vessel by its blood (mm Hg). a. BP always refers to arterial pressure nearest the heart unless otherwise stated b. It is created by pumping action of heart and it decreases steadily the further away the blood gets from pumping action: greatest in aorta (120) and lowest in vena cavas (near zero) b. It is the differences in pressure within the vascular system that keeps blood flowing (greater pressure to lesser pressure). 3. Resistance (R) is the opposition to flow and is a measure of the amount of friction the blood encounters as it passes through the vessels. a. It is often referred to as peripheral resistance since most resistance occurs in systemic circulation 4. There are 3 important sources of resistance: a. Blood viscosity. (Increased viscosity --> increased resistance) b. Vessel length (Increased length --> increased resistance) ** c. Vessel diameter (the smaller the diameter created by vasoconstriction the greater the resistance) 5. The smaller the tube the greater the friction because more fluid is in contact with the walls, hence the increased R 6. Because under normal conditions vessel length and viscosity remain constant, diameter is most important in determining R. 4 7. B. C. Recall arterioles are involved in minute to minute changes in R via sympathetic input and vasodilation/constriction. Relationship Among Flow, Pressure and Resistance 1. Flow is directly proportional to the difference in pressure between 2 points in circulation a. If the difference in pressures is increased, flow is faster b. If the difference is pressures is decreased, flow is slower 2. Flow is inversely proportional to resistance a. If resistance increases (vasoconstriction) flow to the distal organ decreases b. If resistance decreases (vasodilation) flow to the distal organ increases Systemic Blood Pressure 1. Pumping action of heart generates blood flow 2. Pressure results when flow is opposed by resistance 3. Pressure is highest in aorta and declines throughout the length of the pathway 4. Steepest change occurs in arterioles which offer greatest resistance. 5. Venous pressure is steady and gradient from venules to right atrium is only 10 mm Hg because most pressure is dissipated in arterioles. 6. A cut artery spurts blood because of high pressure, but a cut vein give even flow because of low pressure. 7. BP is measured by sphygmomanometer and stethoscope and is expressed as systolic over diastolic pressure. (120/80 mm Hg) 8. Systolic pressure = pressure peak in aorta from expansion during ventricular systole. a. average = 120 mm Hg. 9. Diastolic pressure = lowest pressure in aorta during ventricular diastole. a. average = 70 - 80 mm Hg. Elastic arteries act as axillary pumps that operate throughout diastole because of their recoil properties. --> continuous flow of blood. * 11. Pulse pressure = difference between systolic and diastolic pressures which is felt as throbbing pulsation Maintaining Blood Pressure A. Overview ** 1. BP = CO X PR or BP = SV X HR X PR ** a. Increases in either stroke volume or heart rate --> increased BP (CO = SV X HR). ** b. Increase in PR --> increase BP (increase resistance -decreased flow so blood back up and --> increase BP) 2. Causes for increased HR (review) a. increased sympathetic stimulation 10. VI. 5 B. b. increased epinephrine from adrenal medulla c. increased temp. 3. Causes for increased SV (review) a. increased venous return (Starlings Law) b. increased sympathetic stimulation c. increased epinephrine. 4. Peripheral resistance is single most important factor influencing BP a. Causes for increased PR (1) vasoconstriction (2) increased viscosity. 5. BP is directly proportional to amount of blood in the system. (increased blood volume --> increased BP) a. Important if reduced by hemorrhage or dehydration. b. Salt increases BP by causing fluid retention. 6. BP regulated by neural, chemical, and renal controls which act continuously to modify CO, PR, and BV Short-term Mechanisms: Neural controls 1. Vasomotor center in medulla (different from cardiac centers) integrates BP control a. Sends steady stream of impulses to smooth muscles of vessels so there is nearly always vasoconstriction = vasomotor tone. ** b. increased sympathetic input -->vasoconstriction (esp. in arterioles) --> increased PR --> increased BP c. Decreased sympathetic input--> vasodilation--> decreased PR --> decreased BP. d. The exception to this rule occurs in the skeletal muscles where Ach is released instead of NE such that vasodilation occurs with increased sympathetic input. In times of stress, muscles need more blood not less. 2. Vasomotor center is modified by inputs from baroreceptors, chemoreceptors, higher brain centers, hormones, and other blood borne chemicals. 3. Baroreceptors are sensitive to stretch and detect changes in arterial blood pressure.= BRAKES a. Increased BP --> Increased baroreceptor stretching--> increased sensory input via glossopharyngeal nerve (cranial nerve IX) --> impulses to 3 places: (1) Vasomotor center --> decreased sympathetic output to arterioles --> vasodilation --> decreased PR -> dec. BP. AND (2) Cardioinhibitory center --> increased parasympathetic output via vagus nerve --> Decreased HR --> decreased CO --> dec. BP. AND 6 (3) Cardioacceleratory center to sympathetic input --> decreased CO --> decreased BP b. Function primarily in short term changes such as those occurring with changes in posture. Not effective vs. sustained pressure as seen in chronic c. hypertension. 4. Chemoreceptors in carotid arteries and aortic arch are sensitive to changes in O2 and pH a. Decreased BP --> (1) decreased oxygen, (2) increased carbon dioxide, and (3) decreased pH (increased H+) --> increased chemoreceptor activity --> increased input to vasomotor center --> increased sympathetic input to arterioles ->increased vasoconstriction --> increased PR --> increased BP--> increased speed for blood to get to lungs and tissues. (impulses also sent to Cardioacceleratory and Cardioinhibitory centers) 5. Higher brain centers (cerebral cortex and hypothalamus) modify BP via relays to medullary centers. a. Hypothalamus creates "flight or flight response to increased BP, and redistributes blood during exercise and changes in body temperature. C. Short-term Mechanisms: Chemical controls: 1. Adrenal medulla releases Ne and E during stress a. NE promotes vasoconstriction --> increased BP b. E increased HR and causes general vasoconstriction except in skeletal muscle where it promotes vasodilation to increased O2 supply during exercise. 2. Antidiuretic hormone (ADH) produced by hypothalamus a. Stimulates kidneys to conserve water-->increased BP b. Released in great amounts in hemorrhage and promotes vasoconstriction 3. Alcohol causes drop in BP because it a. Inhibits ADD --> increased water excreted -->decreased in BV --> decreased BP b. depresses vasomotor centers -->vasodilation (decreased BP) especially in skin (alcohol flush). D. Long-term Mechanisms: Renal controls 1. Direct method: When BV or BP rises --> increasedfiltration and therefore increased loss of water from body --> decreased BV and decreased BP 2. Indirect method = renin-angiotensin mechanism a. Decreased BP --> increased in enzyme renin from kidneys (1) formation of angiotensin II--> vasoconstriction --> increased BP. 7 VII. VIII. * Note: angiotensin II is a very powerful vasoconstrictor (2) Angiotensin II also stimulates adrenal cortex to secrete aldosterone -->increased Na+ reabsorption and then water reabsorption from kidneys -->increased blood volume --> increased BP. Alterations in Blood Pressure A. Hypotension 1. Low BP 2. Represented by a systolic pressure < 100 mm Hg 3. Generally associated with long life and an old age free of illness B. Hypertension 1. = High blood pressure: 140/90 or higher 3. A major contributing factor in atherosclerosis, heart attacks, strokes, and renal failure 4. Essential (primary) hypertension = most common (90%) and cause is unknown, but thought to be a disturbance of mechanisms hat regulate BP a. Associated with increased vascular resistance such that heart must pump harder to overcome resistance --> weakens heart over time b. Contributing factors include: (1) diet: one needs to reduce sodium, saturated fat, cholesterol, and weight (2) Age: most common >40 (3) Race: more common in African Americans (4) Heredity (5) Stress (6) Smoking 5. Secondary hypertension occurs as result of some other disorder such as kidney disease, arteriosclerosis and hyperthyroidism a. (if arteries of kidneys are narrowed by disease, kidneys think BP is low --> renin release --> increased angiotensin II and aldosterone --> vasoconstriction and water retention --> increased BV and BP) Blood Flow through Body Tissues A. Velocity of Blood Flow 1. Flow in any vascular component is inversely proportional to the total cross sectional area * a. Increased area --> decreased rate of flow b. Think of a river: speeds up in narrow channels and is slow where it is wide. 2. Capillaries have 600 X the cross-sectional area of aorta, veins have 4 X cross-sectional area of corresponding arteries. a. Velocity greatest in aorta , decreased in arteries and arterioles, lowest in capillaries, speeds up somewhat in veins. 8 IX. b. Large capillary area and slow speed important for diffusion. 3. Remember that although the lumens of the capillaries are small, when all the lumens are added together the volume of blood they can hold is much great than say the aorta B. Autoregulation of Blood Flow 1. Autoregulation is the automatic adjustment of blood flow to each tissue in proportion to its requirements at any point. 2. Regulated by local chemical conditions and independent of systemic factors. C. Metabolic Controls 1. In most tissues declining levels of oxygen = strongest stimulus for vasodilation, but in brain = elevated levels of carbon dioxide and decreased pH. 2. Vasodilation also created locally by metabolically active tissues which secrete K+, H+, lactic acid, prostaglandins, and inflammatory chemicals such as histamine. D. Myogenic (smooth muscle) Controls 1. Increased stretching from elevated BP causes local vasoconstriction to decrease blood flow to organ and decreased stretch from lowered BP causes local vasodilation to increase flow to that organ. E. Long term autoregulation 1. Long-term autoregulation mechanisms kick in if requirements for more blood persists. 2. Solutions include a. an increased # blood vessels, b. Enlargement of existing vessels c. Especially common in heart when coronary vessel partially occluded or in high altitudes. Capillary Dynamics (simplified) A. Review of terms 1. Plasma = fluid portion of blood within blood vessels. 2. Interstitial fluid = fluid derived from the blood that surrounds tissues, i.e., fluid outside blood vessels and body cells. 3. Lymphatic fluid = protein-containing fluid within lymphatic vessels. a. Composed of materials picked up from interstitial fluid for transportation back to the blood vessels. 4. Oxygen, carbon dioxide, most nutrients and metabolic wastes pass between blood and interstitial fluid by diffusion along a concentration gradient. (> to <) 5. Fluid and its dissolved substances are forced out of capillaries at arterial end but most of it returns to blood stream at venous end through the opposing forces of hydrostatic and osmotic pressures. B. Net results 9 1. X. Fluids leave the capillary when CHP is greater than COP and fluids enter the capillary from the interstitial fluid when COP is greater than CHP. 2. Consequently fluid flows out of capillaries at arterial end and flows back into the capillaries at the venous end. 3. That which is not reabsorbed is eventually returned to circulation via the lymphatic system. b. Without this return blood vessels would be empty within 24 hrs. E. Edema 1. = swelling that results from disruption in the normal flow in and out of capillaries such that fluid accumulates in the tissues. 2. 2 categories of causes: a. Increased filtration b. Hindered return 3. Increased filtration may be caused by increased CHP. Caused for increased CHP include: a. high BP b. increase BV as in sodium retention c. congestive heart failure and d. incompetent venous valves 4. Increased filtration may also be caused by increased capillary permeability as seen in: a. burns b. crushing injuries and c. allergic reactions 5. Hindered return may be caused by: a. Starvation where there are insufficient plasma proteins to maintain osmotic pressure in blood or b. kidney disease where there is a loss of proteins in urine such that osmotic pressure cannot be maintained in the blood Cardiovascular disease A. General features 1. 1/4 of all Americans have some form of CV disease 6. Beta blocking agents used to inhibit actions of sympathetic NS -> decreased HR --> decreased CO --> decreased BP B. Atherosclerosis 1. Arteriosclerosis = general term describing any number of conditions in which arteries thicken and lose elasticity. 2. Atherosclerosis = most common form in which fatty deposits of plaque line arteries, especially coronary and cerebral --> MI and cerebral vascular accidents (stroke) 3. Aneurysm = saclike outpocketing of wall of vessel or heart chamber 10 a. XI. Plaque may so damage a vessel it will balloon and eventually burst b. Aorta is most common site: highest BP Circulatory pathways A. Fetal circulation 1. Umbilical vein carries oxygenated blood from placenta into fetus where it is conveyed toward the liver. a. Some goes into liver and then into inferior vena cava b. Some bypasses the liver (because functions of liver already performed by the mother). c. Ductus venosus = shunt which directs blood from umbilical veins directly into inferior vena cava. 2. Umbilical arteries carry blood from the fetus to the placenta for exchange of gases, nutrients, and wastes. 3. 2 bypasses in fetal heart decrease blood flow to lungs whose function is also performed by placenta. a. Foramen ovale is opening between right and left atria. Closes at birth and becomes fossa ovalis b. Ductus arteriosus is shunt between pulmonary trunk and aorta. Closes at birth and becomes ligamentum arteriosum B. Hepatic portal system 1. Unusual in that it is a system with 2 capillary beds. 2. Begins with capillary bed in digestive organs which form veins named for their respective organs (splenic, pancreatic, superior/inferior mesenteric) which join to form the hepatic portal vein which enters liver. 3. In liver the second capillary beds form from which excess food is removed and processed. 4. These beds form veins which dump into hepatic vein which in turn empty into inferior vena cava 11 Abdominal aorta Hepatic A Gastric A Cap in Stomach Pancreatic A Cap. In pancreas Splenic A Capillaries in spleen Gastric V Splenic V Celiac A. Superior mesenteric A Cap in SI Pancreatic V Superior Mesenteric V Hepatic Portal V Capillaries in Liver Renal A Capillaries in Kidney Renal V Hepatic V IVC 12 Right atrium