The Heart: Cardiac Output
advertisement

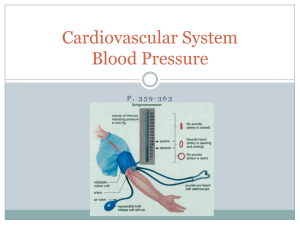
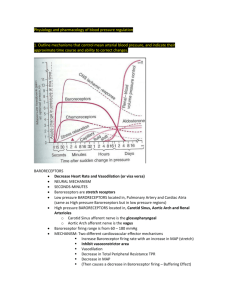
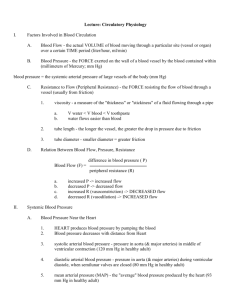
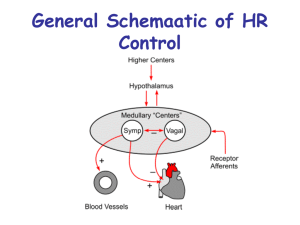
The Heart: Cardiac Output Cardiac output (CO) • Amount of blood pumped by each side of the heart in one minute • The average resting CO for an adult is 3-5 liters pumped per minute • Entire volume passes through body ~ once per minute • CO = (heart rate (beats/min) x stroke volume (Liters/beat) o At rest: CO (ml/min) = HR (75 beats/min) SV (70 ml/beat) = 5.25 L/min o Maximal CO is 4–5 times resting CO in nonathletic people o Maximal CO may reach 35 L/min in trained athletes Stroke volume = Volume of blood pumped by each ventricle in one contraction Regulation of Blood Pressure The main factors influencing blood pressure: • Cardiac output (CO) = Stroke volume x heart rate • Peripheral resistance (PR) Blood pressure = CO x PR • Blood volume (BV) Three Types of Blood Pressure Control • Autoregulatory mechanisms • Metabolic O2 & myogenic control cause vasodilation • Neural mechanisms • Motor centers, chemo- & baroreceptors influence CO • Hormonal mechanisms • Many hormones increase PR through vasoconstriction or through osmoregulation to increase BV Regulation of Blood Pressure The main factors influencing blood pressure: • Cardiac output (CO) • Peripheral resistance (PR) Blood pressure = CO x PR • Blood volume (BV) Three Types of Blood Pressure Control • Autoregulatory mechanisms • Metabolic O2 & myogenic control cause vasodilation • Neural mechanisms • Motor centers, chemo- & baroreceptors influence CO • Hormonal mechanisms • Many hormones increase PR through vasoconstriction or through osmoregulation to increase BV Autoregulatory (Intrinsic) Mechanisms Autoregulation occurs at the local level, in capillary beds of organs and tissues (acidosis) High O2, high pH, high nutrients, low CO2 cause precapillary sphincters to close Low O2, high CO2, low pH, low nutrients cause precapillary sphincters to open (from locally high BP) Regulation of Blood Pressure The main factors influencing blood pressure: • Cardiac output (CO) • Peripheral resistance (PR) Blood pressure = CO x PR • Blood volume (BV) Three Types of Blood Pressure Control • Autoregulatory mechanisms • Metabolic O2 & myogenic control cause vasodilation • Neural mechanisms • Motor centers, baro- & chemoreceptors influence CO • Hormonal mechanisms • Many hormones increase PR through vasoconstriction or through osmoregulation to increase BV Neural Control of Blood Pressure A short-term control mechanism Controls peripheral resistance in two ways • Vasodilation/constriction • Altering blood distribution Brain regulation in the medulla oblongata • Vasomotor center: maintains arteriole tone and receive baro- and chemoreceptor inputs • Cardiac centers: Acceleratory and inhibitory via sympathetic and parasympathetic divisions • VC + CC = Cardiovascular center Cardiac Centers Increase or Decrease Heart Rate BP activates cardiac centers in medulla Parasympathetic activity Sympathetic activity Heart rate (HR) Cardiac output (CO = SV x HR Figure 19.8 Baroreceptor-Initiated Reflexes Baroreceptors (Pressure sensors) • Location: carotid sinuses, aortic arch, walls of large neck and thorax arteries • Increased blood pressure: 1. Stimulates baroreceptors to increase input to the vasomotor center which then: 2. Inhibits the vasomotor center, causing arteriole dilation and venodilation 3. Stimulates the cardioinhibitory center, or parasympathetic (vagus) nerve impulses to turn down heart rate Effects of Baroreceptor Sensing on Cardiovascular Center 3 Impulses from baroreceptors stimulate cardioinhibitory center (and inhibit cardioacceleratory center) and inhibit vasomotor center. 4a Sympathetic impulses to heart cause HR, contractility, and CO. 2 Baroreceptors in carotid sinuses and aortic arch are stimulated. Vasodilation 4b Rate of vasomotor impulses allows vasodilation, causing R BP too high 1 Stimulus: Blood pressure (arterial blood pressure rises above normal range). Homeostasis: Blood pressure in normal range 5 CO and R return blood pressure to homeostatic range. 1 Stimulus: 5 CO and R return blood pressure to homeostatic range. Blood pressure (arterial blood pressure falls below normal range). BP too low 4b Vasomotor fibers stimulate vasoconstriction, causing R Vasoconstriction 2 Baroreceptors in carotid sinuses and aortic arch are inhibited. 4a Sympathetic impulses to heart cause HR, contractility, and CO. 3 Impulses from baroreceptors stimulate cardioacceleratory center (and inhibit cardioinhibitory center) and stimulate vasomotor center. Figure 19.9 Chemoreceptor-Initiated Reflexes Chemoreceptors (Chemical sensors) • Location: carotid sinus, aortic arch, large neck arteries • Respond to rise in CO2, drop in pH or O2 o Increase blood pressure via the vasomotor center and the cardioacceleratory center o Are more important in the regulation of respiratory rate, which also controls blood pH and O2/CO2 levels Regulation of Blood Pressure The main factors influencing blood pressure: • Cardiac output (CO) • Peripheral resistance (PR) Blood pressure = CO x PR • Blood volume (BV) Three Types of Blood Pressure Control • Autoregulatory mechanisms • Metabolic O2 & myogenic control cause vasodilation • Neural mechanisms • Motor centers, baro- & chemoreceptors influence CO • Hormonal mechanisms • Many hormones increase PR through vasoconstriction or through osmoregulation to increase BV Hormonal Mechanism of BP Control Norepinephrine (NE) and epinephrine (Epi) cause generalized vasoconstriction and increase cardiac output BP Atrial natriuretic peptide (ANP) causes blood volume and blood pressure to decline, causes generalized vasodilation BP Antidiuretic hormone (ADH-vasopressin) causes intense vasoconstriction in cases of extremely low BP BP Erythropoietin (EPO) from kidneys increases RBC production, blood pressure (banned in Olympics) BP Angiotensin II, generated by kidney release of renin, causes vasoconstriction BP Kidney Specific Hormonal Mechanisms Baroreceptors quickly adapt to chronic high or low BP Long-term mechanisms step in to control BP by altering blood volume Kidneys act directly and indirectly to regulate arterial blood pressure 1. Direct renal mechanism- elimination or retention of salts and water based on BP and BV 2. Indirect renal (renin-angiotensin) mechanism Renin-Angiotensin Pathway: Indirect Mechanism The renin-angiotensin mechanism • Arterial blood pressure release of renin • Renin production of angiotensin II Ways that Angiotensin II increases BP 1. It is a potent direct vasoconstrictor BP 2. Angiotensin II aldosterone secretion Aldosterone renal reabsorption of Na+ and urine formation, increasing blood volume BV 3. Angiotensin II stimulates ADH release, saving water and Na+ and increasing blood volume BV 4. It reduces blood flow through the kidneys, reducing urine output BV Renin-Angiotensin II Mechanism of Blood Pressure Increase Arterial pressure Indirect renal mechanism (hormonal) Direct renal mechanism Baroreceptors Sympathetic stimulation promotes renin release Reduction of blood flow Kidney Renin release Angiotensin-converting enzyme (ACE) inhibitors are drugs that block angiotensin II production. ACEs are used to treat hypertenion and congestive heart failure. catalyzes cascade, resulting in formation of Angiotensin II Filtration ADH release by posterior pituitary Aldosterone secretion by adrenal cortex Water reabsorption by kidneys Sodium reabsorption by kidneys Blood volume Vasoconstriction ( diameter of blood vessels) Initial stimulus Physiological response Result Arterial pressure Figure 19.10 Summary of Mechanisms Controlling Blood Pressure Activity of muscular pump and respiratory pump Release of ANP Fluid loss from hemorrhage, excessive sweating Crisis stressors: Bloodborne Dehydration, exercise, trauma, chemicals: high hematocrit body epinephrine, temperature NE, ADH, angiotensin II; ANP release Conservation of Na+ and water by kidney Blood volume Blood pressure Blood pH, O2, CO2 Blood volume Baroreceptors Chemoreceptors Venous return Stroke volume Body size Caused by EPO release Activation of vasomotor and cardiac acceleration centers in brain stem Heart rate Cardiac output Diameter of blood vessels Blood viscosity Blood vessel length Peripheral resistance Initial stimulus Physiological response Result Mean systemic arterial blood pressure Figure 19.11 Blood Pressure: Effects of Factors Blood Pressure = Cardiac Output x Peripheral Resistance BP = CO x PR Neural factors • Renal factors • Regulation by altering blood volume: salt and water retention • Renin – hormonal control Temperature • Heat has a vasodilating effect • Cold has a vasoconstricting effect Chemicals • Autonomic nervous system adjustments (sympathetic division): vasoconstriction Various substances can cause increases or decreases Diet • High salt causes elevated BP Comparison of Blood Pressures Blood pressure results when flow is opposed by resistance Disease causing blood pressure change Arteriosclerosis: Hardening of the artery walls and decrease of elasticity, restricting flow and increasing blood pressure. Atherosclerosis: A specific type of arterosclerosis where arteries are clogged by an accumulation of plaques: cholesterol particles (lipoproteins), fat, calcium, cellular waste and other substances. Capillary Exchange: Mechanisms Direct diffusion across plasma membranes Endocytosis or exocytosis Some capillaries have gaps (intercellular clefts) • Plasma membrane not joined by tight junctions Fenestrations of some capillaries • Fenestrations = pores Blood and Osmotic Pressure Drive Transport • Blood pressure is higher than osmotic pressure at the arterial end of the capillary bed; net flow inwards • Osmotic pressure is higher than blood pressure at the venous end; net flow inwards Therefore, fluid moves out of capillaries at the afferent end and into capillaries (reabsorption) at the efferent end