Ch 19 Circulation Physiology
advertisement
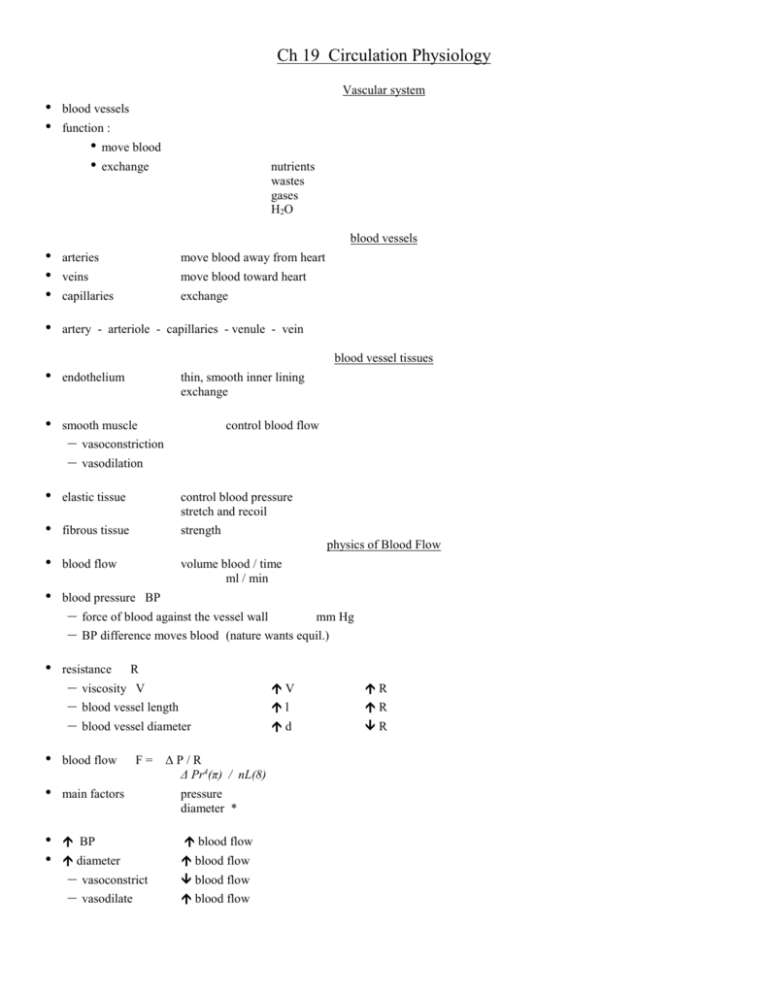
Ch 19 Circulation Physiology Vascular system • • blood vessels function : • move blood • exchange nutrients wastes gases H2O blood vessels • • • • arteries move blood away from heart veins move blood toward heart capillaries exchange artery - arteriole - capillaries - venule - vein blood vessel tissues • endothelium • smooth muscle – – thin, smooth inner lining exchange control blood flow vasoconstriction vasodilation • elastic tissue control blood pressure stretch and recoil • fibrous tissue strength physics of Blood Flow • blood flow • blood pressure BP • – – force of blood against the vessel wall R viscosity V V R blood vessel length l R blood vessel diameter d R • blood flow • main factors pressure diameter * BP blood flow diameter blood flow • • – – mm Hg BP difference moves blood (nature wants equil.) resistance – – – volume blood / time ml / min F= ΔP/R Δ Pr4(π) / nL(8) vasoconstrict blood flow vasodilate blood flow Blood Pressure • • • • • fluid pressure = force exerted by the pump blood pressure = force exerted by heart systolic BP force from left ventricle (systole) blood pushes blood 120+ mm Hg diastolic BP force of elastic walls (recoil) artery wall squeezes blood 80 mm Hg pulse pressure systolic BP - diastolic BP 120 - 80 = 40 mmHg MAP • • • mean arterial pressure – ave. BP in a vessel MAP = diastolic BP + (pulse press / 3) 80 (40 / 3) = 93 mmHg or, (2x diastolic BP + systolic BP)/3 due to: BP varies with stretch and recoil of elastic arteries arterioles have little elasticity – systolic BP = diastolic BP no Pulse Pressure BP drops • • • BP drops throughout the circuit capillary BP – – enter 35 mmHg exit 15 mmHg venous BP – 20 to 0 mmHg venous BP • • rarely varies venous return – – – to R atrium blood pressure respiratory pump inhaling • decreases pressure in thoracic cavity – vacuum • increase pressure abdominal cavity – squeezes abdominal veins skeletal muscle pump • muscles compress veins • squeeze blood forward • valves prevent backflow maintanence of BP • • cardiac output – – CO = SV x HR CO BP SV and/or HR BP peripheral resistance – – vasoconstriction BP viscosity BP • polycythemia, anemia • • blood volume – – volume BP eg. osmolarity, blood loss these compensate for each other to maintain optimum BP regulation of BP • • • • receptors – – baroreceptors chemoreceptors neural control – – medulla and ANS higher brain centers chemical control renal control neural control of BP • • • control peripheral resistance alters blood distribution to organs medulla – – • arterioles vasomotor centers BP BP vasomotor center S-ANS vasodilation vasomotor center S-ANS vasoconstriction vasomotor tone constant, moderate vasoconstriction vasomotor fibers • • • • S-ANS to smooth muscle of blood vessels S-ANS to vessels in skin and organs – norepinephrine vasoconstrict S-ANS to vessels to skeletal muscle – acetylcholine vasodilate exercise - increase blood to skeletal muscles w/o increase BP BP reflex arc • • • • • receptor baroreceptors sensory neuron to medulla integration medulla – vasomotor center motor neuron S-ANS effector blood vessel smooth muscle receptors • • baroreceptors – – – – pressure receptor carotid sinus ; aortic arch stretch stim by BP inhibits vasomotor center S- ANS BP chemoreceptors carotid body ; aortic body – stim by – stim vasomotor center oxygen CO2 or pH BP and speed blood flow higher brain centers • • • hypothalamus limbic system cerebral cortex hormonal control • • • • • • epinephrine BP CO some vasoconstriction norepinephrine BP vasoconstriction ADH BP H2O reabsorption aldosterone BP Na reabsorption atrial natriuretic peptide BP renin-angiotensin Na excretion vasodilation BP vasoconstriction aldosterone, ADH other chemical control • • • • • from blood vessel wall – – – local effects endothelin vasoconstriction (Ca entry) prostaglandin vasoconstricion nitric oxide major vasodilator • stim by acetylcholine, kinins, nitroglycerine histamine vasodilate inflammation bradykinins vasodilate inflammation alcohol vasodilate inhibit ADH nicotine vasoconstrict mimics NE renal control • • • • • • alter blood volume to change BP more long term vs altering resistance maintains blood volume (~ 5 L) and BP by altering amount of urine – – urine - blood volume urine - blood volume bl volume ( BP) - urine - blood volume bl volume ( BP) - urine - blood volume measuring BP • • • • • sphygmomanometer stethoscope auscultation sounds of Korotkoff – not heard when blood flows freely no blood flows systolic pressure 1st sounds heard diastolic pressure sounds stop hypotension • • • below 100 / 60 orthostatic hypotension chronic hypotension – – – age decreased viscosisty Addison’s decreased aldosterone hypothyroid hypertension • • • • above 140 / 90 normal fever , exercise , emotion primary (essential) hypertension – contributing factors – TX: no cause diet , weight , age heredity , smoking , stress diuretics beta blockers Ca channel blockers ACE inhibitors secondary hypertension – – – other disorders kidney Cushing’s Grave’s Blood flow • • tissue perfusion flow of blood through an organ goals of blood flow : – – move blood exchange • exchange at tissue cells – gases – nutrient , wastes • gas exchange at lung • nutrient absorption from digestive tract • blood filtering in kidney velocity of blood flow • • • slows as increase cross-sectional area aorta – smallest area fastest capillaries – – – greatest area slowest WHY? local regulation of blood flow • • • BP controlled systemically blood flow to each organ controlled locally = autoregulation • varying resistance (diameter) of local arterioles • metabolic due to chemical changes • myogenic due to stretch of smooth muscle metabolic autoregulation • • • vasodilation of arterioles leading into capillaries metabolic changes – – – – decreased O2 (hypoxia) nitric oxide H+ (low pH) lactic acid inflammatory chemicals – – histamine kinins myogenic autoregulation • • • • maintains local perfusion stretch smooth muscle causes increased tone local BP (stretch) causes local vasoconstriction local BP (stretch) causes local vasodilation • reactive hyperemia • angiogenesis – – increased blood flow to area of occlusion increased blood vessels if long term hypoxia capillaries • • capillary beds = precapillary sphincters – – network of capillaries smooth muscle at root of each capillary regulate flow into each capillary local control • increase flow if increase needs of tissues capillary permeability • • • • • • • holes – – clefts spaces between cells of capillary fenestrations pores in cell walls of capillary diffusion O2 , CO2 , lipids filtration fluid forced through holes capillary dynamics hydrostatic pressure – = fluid pressure against a wall = capillary Blood Pressure HPc capillary hydrostatic pressure HPif interstitial fluid hydrostatic pressure ~0 net force of fluid out of capillary = HP c – HPif = HPc – – arterial end 35 mmHg venous end 15 mmHg capillary dynamics 2 • • • • • colloid osmotic pressure = plasma proteins (albumin) in blood pull of water into blood = concentration gradient water follows particles OP = 25 mmHg = osmosis colloids capillary dynamics 3 • • • • • net fluid pressure NFP NFP = HP – OP net flow = pressure out – pressure in HP – OP = arterial end: venous end 10 mmHg fluid out -8 mmHg fluid in HP – OP = blood flow to skeletal muscle • • • exercise hyperemia vasodilation autoregulation – vasodilation due to low O2 systemic vasoconstriction – maintain BP and blood flow blood flow to skin • • • temperature regulation hot increase blood flow – hypothalamus decreased vasomotor stimulation relax smooth muscle vasodilation – local release nitric oxide = vasodilation cold decrease blood flow blood flow to brain • • • • • • requires constant blood flow – 750 ml / min high nutrient needs low pH ; high CO2 vasodilation ; increase flow low O2 vasodilation high CO2 (hyperventilate) depress brain activity lose control of flow BP vasodilate – to maintain flow BP vasoconstrict – to prevent rupture blood flow to lungs • • low pressure circuit 24 / 8 autoregulation reversed – – low O2 vasoconstrict high O2 vasodilate blood flow to heart • • • • coronary arteries flow to myocardium during diastole only low O2 vasodilation exercise vasodilation